
ARTICLE doi:10.1038/nature19830 The MCL1 inhibitor S63845 is tolerable and effective in diverse cancer models
András Kotschy1, Zoltán Szlavik1, James Murray2, James Davidson2, Ana Leticia Maragno3, Ga?tane Le Toumelin-Braizat3,
Ma?a Chanrion3, Gemma L. Kelly4,5, Jia-Nan Gong4,5, Donia M. Moujalled6, Alain Bruno3, Márton Csekei1, Attila Paczal1,
Zoltán B. Szabo1, Szabolcs Sipos1, Gábor Radics1, Agnes Proszenyak1, Balázs Balint1, Levente Ondi1, Gábor Blasko1,
Alan Robertson2, Allan Surgenor2, Pawel Dokurno2, Ijen Chen2, Natalia Matassova2, Julia Smith2, Christopher Pedder2, Christopher Graham2, Aurélie Studeny3, Ga?lle Lysiak-Auvity3, Anne-Marie Girard3, Fabienne Gravé3, David Segal4,5,
Chris D. Riffkin4,5, Giovanna Pomilio6, Laura C. A. Galbraith4,5, Brandon J. Aubrey4,5,7, Margs S. Brennan4,5, Marco J. Herold4,5, Catherine Chang4,5, Ghislaine Guasconi3, Nicolas Cauquil3, Fabien Melchiore8, Nolwen Guigal-Stephan8, Brian Lockhart8,
Frédéric Colland3, John A. Hickman3, Andrew W. Roberts4,5,7,9, David C. S. Huang4,5, Andrew H. W ei6,10, Andreas Strasser4,5, Guillaume Lessene4,5,11 & Olivier Geneste3
Apoptosis is an evolutionarily conserved process of programmed cell death that is essential for the elimination of unwanted or potentially dangerous cells1. Avoidance of apoptosis is critical for the development and sustained expansion of tumours and underpins resistance to diverse anti-cancer treatments2. BCL-2 family proteins are key r egulators of the mitochondrial apoptotic pathway and are characterized by the presence of at least one of four BCL-2 homology (BH) domains. They comprise a pro-survival group (BCL-2, BCL-X L, BCL-W, MCL1 and BFL1, also known as BCL2A1) and two pro-apoptotic subgroups: the multi-BH domain cell death effectors (BAX, BAK and BOK) and the BH3-only apoptosis initiators (for example, BIM and BAD)3. Interactions among these subgroups, involving binding of the BH3 domain of the pro-apoptotic members to a groove on the surface of the pro-survival proteins, controls commitment to apoptosis4. In many cancers, the balance between the pro- and anti-apoptotic BCL-2 family members is tipped towards survival as a consequence of genetic or epigenetic changes5.
The promising clinical activity of small molecule inhibitors t argeting BCL-2, BCL-X L and BCL-W (navitoclax, ABT-263)6,7 or BCL-2 alone (venetoclax, ABT-199)8 has validated the use of BH3-mimetic drugs to directly activate apoptosis in cancers9. MCL1 gene amplifications are frequently found in human cancers10 and several key o ncogenic pathways lead to increased MCL1 protein expression through transcriptional or post-transcriptional mechanisms11. Studies using inducible gene deletion, RNA interference or inducible expression of ligands that inhibit distinct pro-survival BCL-2 family members have shown that MCL1 is essential for the growth of diverse tumours, including acute myeloid leukaemia (AML)12, MYC-13 or BCR–ABL-driven pre-B or B lymphomas14, T cell lymphomas15,16, multiple myeloma17, certain breast cancers and non-small-cell lung carcinoma (NSCLC) cell lines carrying MCL1 gene amplifications10. Certain com-pounds that broadly inhibit gene transcription (for example, anthra-cyclines and CDK9 inhibitors) or protein translation (for example, puromycin and emetine) are thought to exert their cytotoxic effects in tumour cells, at least in part, by downregulating MCL1 (ref. 18).
No drug-like MCL1 inhibitors have been published yet; the only compounds showing on-target activity are of weak cellular potency and therefore useful only as in vitro chemical tools19–21. Moreover, conditional gene knockout studies have shown that MCL1 is essential for the survival of haematopoietic stem cells22, cardiomyocytes23,24 and several other critical cell types3, raising the issue of tolerability when targeting MCL1.
In this paper, we describe the development and mechanism of action of S63845, a potent, selective MCL1 inhibitor. S63845 exhibited low nanomolar cytotoxic activity in multiple cancer-derived cell lines in vitro and potent efficacy in vivo in preclinical mouse models of diverse haematological malignancies. The ability of normal tissues in mice to tolerate doses of S63845 that efficiently kill tumour cells i ndicates that a suitable therapeutic window may be achievable for MCL1-specific BH3 mimetics.
Avoidance of apoptosis is critical for the development and sustained growth of tumours. The pro-survival protein myeloid cell leukemia 1 (MCL1) is overexpressed in many cancers, but the development of small molecules targeting this protein that are amenable for clinical testing has been challenging. Here we describe S63845, a small molecule that specifically binds with high affinity to the BH3-binding groove of MCL1. Our mechanistic studies demonstrate that S63845 potently kills MCL1-dependent cancer cells, including multiple myeloma, leukaemia and lymphoma cells, by activating the BAX/ BAK-dependent mitochondrial apoptotic pathway. In vivo, S63845 shows potent anti-tumour activity with an acceptable safety margin as a single agent in several cancers. Moreover, MCL1 inhibition, either alone or in combination with other anti-cancer drugs, proved effective against several solid cancer-derived cell lines. These results point towards MCL1 as a target for the treatment of a wide range of tumours.
1Servier Research Institute of Medicinal Chemistry, Budapest 1031, Hungary. 2Vernalis (R&D) Ltd., Cambridge CB21 6GB, UK. 3Institut de Recherches Servier Oncology R&D Unit, Croissy Sur Seine 78290, France. 4The Walter and Eliza Hall Institute of Medical Research, Melbourne 3052, Australia. 5Department of Medical Biology, University of Melbourne, Melbourne 3010, Australia.
6Australian Centre for Blood Diseases, Monash University, Melbourne 3004, Australia. 7Department of Clinical Haematology and Bone Marrow Transplantation, The Royal Melbourne Hospital, Victorian Comprehensive Cancer Centre, Melbourne 3050, Australia. 8Institut de Recherches Servier, Biomarker Research Division, Croissy Sur Seine 78290, France. 9Faculty of Medicine, The University of Melbourne, Melbourne 3010, Australia. 10Department of Clinical Haematology, The Alfred Hospital, Melbourne 3004, Australia. 11Department of Pharmacology and Pharmaceutics, The University of Melbourne, Melbourne 3010, Australia.
00M O N T H2016|V O L000|N A T U R E|1
2 | N A T U R E | V O L 000 | 00 M O N T H 2016
Highly selective and potent binding of S63845 to MCL1
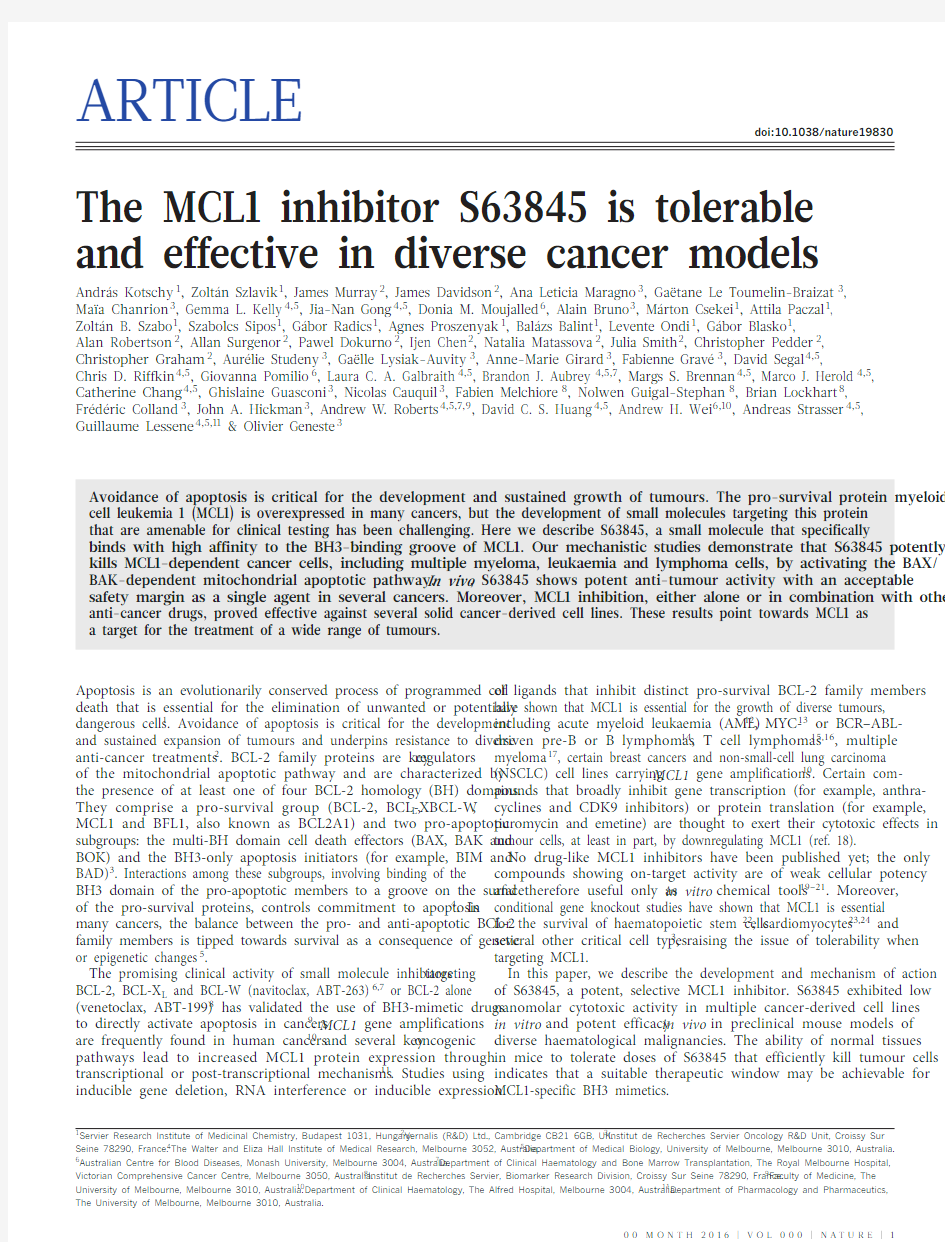
An NMR-based fragment screen and subsequent structure-guided drug discovery yielded S63845 (Fig. 1a), a selective and potent MCL1
i nhibitor. S63845 binds human MCL1 with a K D of 0.19 nM (surface plasmon resonance) and mouse MCL1 with an around 6-fold lower affinity, with no appreciable binding to BCL-2 or BCL-X L (Fig. 1a and Extended Data Fig. 1a). For comparison, A-1210477, a previously
p ublished MCL1 inhibitor 19, has an approximately 20-fold lower
a ffinity for human MCL1 (Extended Data Fig. 1b, c).The BH3-binding grooves on the surfaces of pro-survival BCL-2 family members have common features, most notably the presence of four hydrophobic pockets (P1–P4), which interact with four conserved hydrophobic residues on the BH3 α -helix of the pro-apoptotic BCL-2
family members 25
. The co-crystal structure of S63845 bound to MCL1 revealed that this inhibitor binds to the BH3-binding groove of MCL1 in a site similar to that at which previously published BH3 mimetics were shown to bind 20,26 (Fig. 1b and Extended Data Table 1). The car-boxylate moiety forms a strong interaction with Arg263, an anchor point typical for inhibitors of pro-survival BCL-2 family members 3. The
aromatic scaffold is embedded into the hydrophobic pocket P2 while the terminal trifluoromethyl moiety stretches across into P4, sitting in a small hydrophobic pocket.
S63845 kills tumour cells by BAX/BAK-mediated apoptosis
S63845 was tested alongside other BH3 mimetics (ABT-263 and ABT-199) for its ability to induce apoptosis in three cancer-derived cell lines with known dependency on distinct pro-survival BCL-2 family m embers. S63845 potently killed MCL1-dependent H929 multiple myeloma cells 27, whereas ABT-263 and ABT-199 had only minimal impact (Fig. 1c). S63845 was approximately 1,000-fold more potent in killing H929 cells than the previously described MCL1 i nhibitor A-1210477 (Fig. 1c). This difference in potency is p robably because of the weaker affinity of A-1210477 for MCL1 (Extended Data Fig. 1b), as well as because of binding of A-1210477 to serum proteins, which reduces its bioavailability. Conversely, the a ctivity of S63845 was not affected by serum concentration (Extended Data Fig. 1d). S63845 had little impact on the viability of BCL-2- and BCL-X L -dependent H146 small-cell lung carcinoma cells 28 (Fig. 1c). The sensitivity of RS4;11 l eukaemic cells to S63845 and ABT-199 (Fig. 1c) indicates that this cell line depends on both BCL-2 (ref. 29) and MCL1. The MCL1 d ependence of H929 cells for their survival
was confirmed by using an inducible CRISPR/Cas9 knockout system 30
to target each of the pro-survival BCL-2 proteins (Extended Data Fig. 2).
Selective targeting of MCL1 by S63845 was confirmed by co- immunoprecipitation experiments, which showed that S63845 disrupted binding of BAK and BAX to MCL1 in HeLa cells, whereas it had no impact on the interaction of these pro-apoptotic proteins with BCL-X L or BCL-2 (Extended Data Fig. 3a). Treatment with S63845 increased MCL1 protein levels in the HCT-116 colon carcinoma cell line more potently than treatment with A-1210477 (Fig. 1d; see also ref. 19). The increased MCL1 protein levels were not accompanied by an increase in MCL1 mRNA levels, but correlated with protein half-life extension (Extended Data Fig. 3b–e).
S63845 rapidly induced caspase-dependent phosphatidyl-serine exposure (Fig. 1e), poly ADP-ribose polymerase (PARP) cleavage (Extended Data Fig. 4a), and cytochrome c release from mitochon-dria (Extended Data Fig. 4b), which are all hallmarks of apoptosis, in H929 cells and other cell lines (Extended Data Fig. 4c). BAX- and BAK-deficient H929 cells were resistant to S63845 (Fig. 1f), d emonstrating that S63845 kills cancer cells through on-target activity, that is,
a ctivation of the BAX/BAK-dependent mitochondrial apoptotic
p athway by direct inhibition of MCL1.Activity of S63845 in haematological malignancies
Many multiple myeloma cell lines express high levels of MCL1 and some have been reported to be dependent on MCL1 for survival 31,32. We found that 17 out of 25 multiple myeloma cell lines tested were highly sensitive to S63845 (IC 50 <0.1 μ M ), six lines were moderately sensitive (0.1 μM 1 μM ) (Fig. 2a). The killing activity of S63845 in these cells correlated with the impact of the BIM2A peptide, which specifically inhibits MCL1 (ref. 33), or genetic deletion of MCL1 (ref. 17) but did not correlate with the impact of the BIM–BAD peptide, which inhibits BCL-2, BCL-X L and BCL-W (ref. 34) (Extended Data Fig. 5a, b). The dependence of the killing activity of S63845 on BAX and BAK was confirmed by CRISPR/Cas9 genome editing in two highly sensitive multiple myeloma cell lines (Extended Data Fig. 5c). All multiple myeloma cell lines tested expressed r eadily detectable levels of MCL1 but the most sensitive ones had barely detectable levels of BCL-X L (Extended Data Fig. 5d). In contrast to the BCL-2 inhibitor, multiple myeloma cell lines sensitive to S63845 were not restricted to those carrying a t(11;14) chromosomal translocation 35, but also included ones carrying chromosomal translocations a ssociated with poor prognosis, such as t(4;14) (ref. 36), or TP53 mutations
P2
P4
A r g 263
a
S63845
K I (MCL1, FP) < 1.2 nM K D (MCL1, SPR) = 0.19 nM K I (BCL2, FP) > 10,000 nM K I (BCL-X L , FP) > 10,000 nM
N
N
S
O
F O
HO
O
Cl
O
N
N
O
N
N
CF 3b
ABT -263ABT -199
A-1210477
c
I C 50 (n M , l o g 10)
S63845Actin
BCL-X L
MCL11 n M 3 n M 30 n M 100 n M 300 n M 3,000 n M 10,000 n M
10 n M 1,000 n M S 63845
d
40 kD 30 kD 40 kD
40 kD
30 kD 40 kD
C o n t r o l A -1210477
3,000
30
30
3
C
o n t
r o l
P e r c e n t a n n e x i n V +
Compound concentration (nM)e sgEV
S63845 (μM)
–/–,BAK –/–
P e r c e n t P I e
x c l u d e d c e l l s
0.0
01
0.
01
0.1
1
10
T
A X –/–,
B A K –/–
f
1 n M 3 n M 30 n M 100 n M 300 n M 3,000 n M 10,000 n M
10 n M 1,000 n M C o n t r o l Figure 1 | S63845 binds to the BH3-binding groove of MCL1 and kills tumour cell lines by inducing BAX/BAK-dependent apoptosis.
a , Structure of the MCL1 inhibitor, S63845 with binding affinities (nM) for human MCL1, BCL-2 and BCL-X L (see source data). FP , Fluorescence polarization and SPR, surface plasmon resonance.
b , Structure of S63845 in complex with MCL1. MCL1 is shown as a surface representation
(C and H atoms in grey, O in red, N in blue and S in yellow), the ligand as a stick representation (C and H atoms in green, O in red, N in blue, Cl in green, F in blue–grey and S in yellow). The P2 and P4 hydrophobic pockets and the conserved Arg263 are shown. c , Cellular activity of S63845 and other BH3 mimetics in H929, H146 and RS4;11 human tumour-derived cell lines. Mean ± s.e.m.of n = 3– 8 biological replicates are shown (see source data). d , Western blot analysis of MCL1 and BCL-X L protein levels in HCT-116 cells treated with S63845 or A-1210477. e , Apoptosis induction in H929 cells treated with the MCL-1 inhibitor, S63845, with or without further addition of the caspase inhibitor, QVD-OPh. Mean and individual data points from n = 3 biological replicates are shown (see source data). f , BAX and BAK dependency for S63845 induced killing in H929 cells, as indicated by propidium iodide exclusion assay. Individual data points shown from n = 2 (sgEV , single guide RNA empty vector) or n =3(Bak ?/?,Bax ?/?) biological replicates (see source data). Western blot showing protein expression levels of BAK and BAX. For gel source images, see Supplementary Fig. 1.
00 M O N T H 2016 | V O L 000 | N A T U R E | 3
(Fig. 2a). This suggests that MCL1 inhibitors may be effective in cases refractory to standard-of-care agents.
Intravenously injected (i.v.) S63845 exerted dose-dependent anti- tumour activity in human multiple myeloma (H929 and AMO1)
x enografts in immunocompromised mice (Fig. 2b and Extended Data Fig. 6a), with maximal tumour growth inhibition (TGI max ) of
114% in the AMO1 model and 103% in the H929 model. At 25 mg kg ?1
, S63845 induced complete regression in 7 out of 8 of the mice at 100 days after treatment in the AMO1 model (Extended Data Fig. 6b). Notably, even at the highest tested efficacious dose (independent of the number of administrations), S63845 was well tolerated by the mice with no s ignificant weight loss observed (Extended Data Fig. 6c, d).
S63845 was next tested in a panel of 11 cell lines representative of human lymphomas and chronic myeloid leukaemia (CML; Fig. 2c): five lines were highly sensitive (IC 50 <0.1 μ M ), three were moderately sensitive (0.1 μM 1 μ M ). S63845 also showed potent cytotoxic activity against seven out of seven c-MYC-driven human Burkitt lymphoma cell lines (Extended Data Fig. 6e). These findings are consistent with the MCL1 dependence of c-MYC- or BCR–ABL-driven human and mouse
m alignant cells revealed by inducible MCL1 gene deletion or MCL1 blockade by BIM2A (refs 13, 14).
The in vivo activity of S63845 was tested in the c-MYC-driven mouse lymphoma (lymphomas from E μ-Myc transgenic mice) model, in which both the tumour cells and the normal tissues express mouse MCL1 protein and thus have the same affinity for the drug. All E μ-Myc lymphoma cell lines tested were sensitive to S63845 in vitro with IC 50 ranging from 161 nM to 282 nM (Fig. 2d). Treatment with 25 mg kg ?1 S63845 (i.v.) for five consecutive days was able to cure 70% of i mmuno-competent C57BL/6 mice bearing E μ-Myc mouse l ymphomas (Fig. 2e and Extended Data Fig. 6f, g), with no side-effects evident in normal tissues.The activity of S63845 was next evaluated in a panel of eight AML cell lines: all lines were sensitive to S63845 (IC 50 4–233 nM, Fig. 3a), consistent with results obtained in animal models of AML (ref. 12). No correlation between the potency of S63845 and MCL1 mRNA expres-sion was observed in the combined panel of haematological cancer cell lines (data not shown). However, after investigating the expression of additional BCL-2 family members or even in an unbiased analysis, we found an inverse correlation between sensitivity to S63845 and BCL-X L mRNA expression levels (Fig. 3b and Extended Data Fig. 7a). Accordingly, the five CML cell lines, which expressed comparatively high levels of BCL-X L mRNA, were relatively insensitive to S63845 (IC 50 >1 μM ). In vivo , S63845 showed potent activity in the MV4-11 human AML xenograft model, with a TGI max of 86% at 12.5 mg per kg body weight (Fig. 3c). At 25 mg kg ?1, complete remission was observed in 6 out of 8 mice after 80 days.
To investigate the potential for MCL1 targeting in primary AML, 25 freshly derived patient AML samples were treated with S63845 alongside ABT-199, and the standard-of-care drugs, idarubicin and ara-C (Extended Data Fig. 7b). LC 50 values for S63845 were in the low- nanomolar range in 5 out of 25 cases (20%). Although some S63845-sensitive AML samples were also sensitive to ABT-199, others were selectively sensitive only to S63845 or ABT-199 (Extended Data Fig. 7b). The LC 50 for S63845 was below 1 μM for 3 out of 5 AML cases with adverse cytogenetic karyotypes. The AML samples displayed a wide range of responses to the MCL1 inhibitor, with the most sensi-tive cases requiring 100- to 1,000-fold less S63845 for effective killing
than the resistant ones or normal CD34+
progenitor cells (Fig. 3d). In clonogenic assays, a subset of primary AML samples were sensitive to 100 nM S63845, whereas normal human CD34+ progenitor cells were resistant to this dose (Extended Data Fig. 7c). By contrast, the
s tandard-of-care chemotherapeutic drugs were toxic to clonogenic growth of both leukaemic and normal progenitor cells (Extended Data Fig. 7c).
a
CCND1t(11;14)MMSET/FGFR3
t(4;14)C-MAF t(14;16)
Unknown
S 63845 I C 50 (μM )
Days after treatment initiation
T u m o u r v o l u m
e (m m 3)
b
d
S 63845 I C 50 (μM )
S63845 treatment: day 5, 6, 7, 8, 9 after transplant
50
100Time (days after transplant)
P e r c e n t s u r v i v a l
Vehicle n = 48 (6)
S63845 25 mg kg –1 n = 41 (6)
****P < 0.0001
e
c
S 63845 I C 50 (μM )
Lymphomas
CML
M A F B t (20;22)M A F B t (14;20)t (12;14)
C C N
D 3 t (6;14)K M S -12-B X G M O L P K M S -12-P U 266B H 92K M S -28-B O P M -L P K M S -1K M S -2K M S -3K M S -28-P M M 1J J N -R P M I 822M M 1A N B L K M M -L -36
E J A M O O C I -M Y W L -A R H 756M R E 72B R E 96A H 15A
F 47R A J H M I N S U -D H L -W S U -D L C L S U -93S U -D H L -H U T -7K M -H D a u d K C L -2E M -K -56M E
G -0J U R L -M K Figure 2 | S63845 is effective against haematological cancer-derived cell lines in vitro and in vivo . a , Viability of 25 multiple-myeloma-derived cell lines treated with S63845 (sensitive cell lines in red, IC 50 <0.1μM ; moderately sensitive cell lines in blue, 0.1 μM 1μ M ). Cell lines are grouped according to their characteristic cytogenetic abnormalities. The p53 status is indicated (* , mutated; #, wild type; ?, unknown). Data from n =2–5biological replicates and mean ± s.d. are shown (see source data). b , Anti-tumour effect of S63845 in AMO1 multiple myeloma xenograft model. Mean ± s.e.m. tumour volumes of eight animals per treatment group are shown (* * * P < 0.001 compared to vehicle). For tumour source data, see Supplementary Fig. 2. c , Viability of lymphoma- or chronic-myeloid-leukaemia (CML)-derived cell lines treated with S63845 (sensitive cell
lines in red, IC 50 <0.1μ
M ; moderately sensitive cell lines in blue, 0.1 μM 1μM ).Mean IC 50 and individual data points from n = 2 biological replicates are shown (see source data). d , Viability of E μ-Myc mouse lymphoma cell lines treated with S63845. Mean IC 50 and individual data points from n =3biological replicates are shown (see source data). e , Survival curves of C57BL/6–LY5.1 mice transplanted with E μ-Myc lymphoma cells treated with S63845 or vehicle. Statistical analysis was performed by Mantel–Cox test.
4 | N A T U R E | V O L 000 | 00 M O N T H 2016
Activity of S63845 in solid tumours
S63845 cytotoxic activity was also tested in a panel of solid-tumour- derived cell lines. Although the majority were relatively resistant to S63845 when used as a single agent (IC 50 >1 μ M ), a few cell lines were moderately sensitive with IC 50 <1 μ M in 3 out of 20 NSCLCs, 3 out of 9 breast cancers and 3 out of 12 melanomas (Extended Data Fig. 8a). While there was no clear correlation with the mutational status of these cell lines, investigation of the expression of BCL-2 family m embers and of an unbiased analysis revealed that sensitivity to the MCL1 i nhibitor was inversely correlated with BCL-X L mRNA expression levels (Extended Data Fig. 8b, c). This is consistent with previously published work using MCL1 knockdown 10,37,38.
We next investigated whether solid-cancer-derived cell lines could be sensitized to S63845 by co-treatment with drugs that target onco-genic kinases 39. S63845 was tested in combination with lapatinib (HER2 inhibitor) in the HER2-amplified BT-474 breast-cancer cell line, tarceva (EGFR inhibitor) in the PC9 (EGFR-mutated) NSCLC cell line, trametinib (MEK inhibitor) in SK-MEL-28 (B-RAF-mutated) and SK-MEL-2 (N-RAS-mutated) melanoma cell lines or vemurafenib (RAF inhibitor) in the B-RAF mutated A2058 melanoma cell line. Even though these inhibitors of oncogenic kinases increased the levels of BIM (Extended Data Fig. 8d), they elicited a predominantly cyto-static effect in the cancer cell lines tested (Fig. 4 and Extended Data Fig. 8e). Notably, the combination of these kinase inhibitors with the
MCL1 inhibitor S63845 induced a potent cytotoxic response (Fig. 4 and Extended Data Fig. 8e). These results are consistent with p revious reports showing that inhibitors of oncogenic kinases can potently sensitize tumour cells to BH3-mimetic drugs targeting BCL-2 and/or BCL-X L (refs 40,41).
S63845 is tolerated in mice at efficacious doses
Finally, we investigated the impact of S63845 treatment on key organs and as multiple blood-cell subsets at the dose of 25 mg kg ?1, which is highly efficacious against mouse tumours (Fig. 2e and Extended Data Fig. 6f, g). This dose caused only a minor reduction in certain leukocyte subsets and no histomorphological changes were observed in the liver, heart, kidney, skeletal muscle and other organs of mice (Fig. 5 and Extended Data Fig. 9a, b). C57BL/6 mice could even tolerate a 40 mg per kg body weight dose (Extended Data Fig. 9c). At the dose-limiting level of 60 mg kg ?1, S63845 caused a marked reduction in erythrocytes (Extended Data Fig. 9d) and the mice presented with apathy, weight loss and signs of haemolysis. The fact that S63845 is well tolerated at therapeutically efficacious doses in mouse cancer models contrasts with previous work showing that conditional MCL1 gene targeting has a severe detrimental impact on multiple cell types, often having a fatal outcome 22–24. The most likely explanation is that irreversible loss of MCL1, resulting from gene knockout, is not equivalent to intermittent periods of pharmacological MCL1 inhibition. It is also possible that additional roles of MCL1, independent of its anti-apoptotic function 42, may only be revealed by gene knockout but not by a pharmacological inhibitor.
Conclusion
Here we describe a highly potent and selective small-molecule i nhibitor of the pro-survival protein MCL1 that has noteworthy single agent in vitro and in vivo anti-tumour activity in cancer-derived cell lines known to be MCL1 dependent, while sparing normal tissues at efficacious doses. We confirmed the broad therapeutic applicability of MCL1 inhibition across panels of multiple myeloma, lymphomas, leukaemias and primary AML cells. We show that the therapeutic potential of MCL1 inhibitors extends to several solid tumour models, some of which showed sensitivity to S63845 monotherapy, while many others were only killed when treated with a combination of S63845 and inhibitors of oncogenic kinases. Mechanism-of-action studies confirmed that this MCL1 inhibitor induces hallmarks of apoptosis and kills cancer cells in a manner dependent on pro-apoptotic BAX and/or BAK.
This study presents preclinical evidence that MCL1 is a druggable target and that direct pharmacological inhibition of MCL1 with a BH3-mimetic drug can be tolerated and efficacious against several cancer types. Despite previous work showing that genetic loss of MCL1 causes severe defects in mice, our results suggest that a robust anti-tumour effect and a suitable therapeutic window are achievable with a BH3-mimetic drug that targets MCL1.
a
S 63845 I C 50 (μM )
Time after treatment initiation (days)
T u m o u r v o l u m e (m m 3)
–1–1–1c b
S63845 –pIC 50
B C L -X L e x p r e s s i o n L o g 2(F P K M +0.1)
AML
n = 24
V i a b l e c e l l s %,n o r m a l i z e d t o D M S O
d
M O L M -13M V 4;11N O M O -1T H P -1K G -1P L -21H L -60O C I -A M L 2
0.
00
1
0.
01
0.1
1
10
D M S O
S63845 (μM)
Figure 3 | S63845 is effective against AML samples in vitro and in vivo , but does not readily kill normal human haematopoietic progenitor cells. a , Viability of AML-derived cell lines treated with S63845 (sensitive cell lines in red, IC 50 <0.1μ M ; moderately sensitive in blue, 0.1 μM
BCL-X L mRNA expression levels on the sensitivity of 24 haematological cancer-derived cell lines to S63845 (IC 50 values from Figs. 2c and 3a). DLBCL, diffuse large B cell lymphoma; FPKM, fragments per kilobase per million mapped fragments. The FPKM value is log 2(FPKM +0.1)to account for values of zero. BCL-X L mRNA expression levels (RNA-seq) were extracted from the CCLE database (see source data). The Pearson correlation coefficient and P value are indicated. pIC50 =?l og 10(IC 50) in mol l ?1. c , Anti-tumour activity of S63845 in the MV4-11 AML xenograft model. Mean ± s.e.m. tumour volumes of eight animals per treatment group are shown (* * * P < 0.001 compared to vehicle). For tumour source
data, see Supplementary Fig. 2. d , Comparison of S63845 activity against primary AML samples relative to healthy CD34+ donor cells. The viability of primary AML cells and normal CD34+ cells (from four healthy human donors, red dashed lines) normalized to vehicle control after 48-h exposure to S63845 (in μ M ) are shown (see source data). The mean viability of vehicle-treated primary AML cells after 48-h exposure was 85% (range, 70–97%).
S63845 100 nM Lapatinib 100 nM S63845 300 nM PLX4032 300 nM
S63845 1 μM Days
C e l l p r o l i f e r a t i o n
Days
Trametinib 30 nM
S63845 30 nM Days
Days Tarceva 100 nM
S63845Combination
Drug
Figure 4 | Activity of S63845 against solid-tumour-derived cell lines in vitro with or without other targeted agents. Cell lines were treated with S63845 with or without the MEK1/2 inhibitor, trametenib (SK-MEL-2), the HER-2 inhibitor, lapatinib (BT-474), the B-RAF inhibitor, PLX-4032 (A2058) or the EGFR inhibitor, tarceva (PC-9). Data are normalized to baseline cell survival at the time of initial drug treatment (day 0). Mean and individual data points from three biological replicates are shown (see source data).
00 M O N T H 2016 | V O L 000 | N A T U R E | 5
Online Content Methods, along with any additional Extended Data display items and Source Data, are available in the online version of the paper; references unique to these sections appear only in the online paper.Received 19 July; accepted 7 September 2016. Published online 19 October 2016.
1. Green, D. R. & Llambi, F. Cell death signaling. Cold Spring Harb. Perspect. Biol . 7,
1–24 (2015).
2. Hanahan, D. & Weinberg, R. A. Hallmarks of cancer: the next generation. Cell
144, 646–674 (2011).
3. Czabotar, P . E., Lessene, G., Strasser, A. & Adams, J. M. Control of apoptosis by
the BCL-2 protein family: implications for physiology and therapy. Nat. Rev. Mol. Cell Biol . 15, 49–63 (2014).
4. Petros, A. M. et al. Rationale for Bcl-x L /Bad peptide complex formation from
structure, mutagenesis, and biophysical studies. Protein Sci . 9, 2528–2534 (2000).
5. Delbridge, A. R. D., Grabow, S., Strasser, A. & Vaux, D. L. Thirty years of BCL-2:
translating cell death discoveries into novel cancer therapies. Nat. Rev. Cancer 16, 99–109 (2016).
6. Wilson, W. H. et al. Navitoclax, a targeted high-affinity inhibitor of BCL-2, in
lymphoid malignancies: a phase 1 dose-escalation study of safety,
pharmacokinetics, pharmacodynamics, and antitumour activity. Lancet Oncol . 11, 1149–1159 (2010).
7. Roberts, A. W. et al. Substantial susceptibility of chronic lymphocytic leukemia
to BCL2 inhibition: results of a phase I study of navitoclax in patients with relapsed or refractory disease. J. Clin. Oncol. 30, 488–496 (2012).
8. Roberts, A. W. et al. Targeting BCL2 with venetoclax in relapsed chronic
lymphocytic leukemia. N. Engl. J. Med . 374, 311–322 (2016).
9. Juin, P ., Geneste, O., Gautier, F., Depil, S. & Campone, M. Decoding and
unlocking the BCL-2 dependency of cancer cells. Nat. Rev. Cancer 13, 455–465 (2013).
10. Beroukhim, R. et al. The landscape of somatic copy-number alteration across
human cancers. Nature 463, 899–905 (2010).
11. Akgul, C. Mcl-1 is a potential therapeutic target in multiple types of cancer.
Cell. Mol. Life Sci. 66, 1326–1336 (2009).
12. Glaser, S. P . et al. Anti-apoptotic Mcl-1 is essential for the development and
sustained growth of acute myeloid leukemia. Genes Dev . 26, 120–125 (2012).
13. Kelly, G. L. et al. Targeting of MCL-1 kills MYC-driven mouse and human
lymphomas even when they bear mutations in p53. Genes Dev . 28, 58–70 (2014).
14. Koss, B. et al. Requirement for antiapoptotic MCL-1 in the survival of
BCR–ABL B-lineage acute lymphoblastic leukemia. Blood 122, 1587–1598 (2013).
15. Grabow, S., Delbridge, A. R., Valente, L. J. & Strasser, A. MCL-1 but not BCL-X L is
critical for the development and sustained expansion of thymic lymphoma in p53-deficient mice. Blood 124, 3939–3946 (2014).
16. Spinner, S. et al. Re-activation of mitochondrial apoptosis inhibits T-cell
lymphoma survival and treatment resistance. Leukemia 30, 1520–1530 (2016).
17. Gong, J.-N. et al. Hierarchy for targeting pro-survival BCL2 family proteins in
multiple myeloma: pivotal role of MCL1. Blood blood-2016-03–704908 (2016).
18. Wei, G. et al. Chemical genomics identifies small-molecule MCL1 repressors
and BCL-X L as a predictor of MCL1 dependency. Cancer Cell 21, 547–562 (2012).
19. Leverson, J. D. et al. Potent and selective small-molecule MCL-1 inhibitors
demonstrate on-target cancer cell killing activity as single agents and in combination with ABT-263 (navitoclax). Cell Death Dis . 6, e1590 (2015).
20. Pelz, N. F. et al. Discovery of 2-indole-acylsulfonamide myeloid cell leukemia 1
(Mcl-1) inhibitors using fragment-based methods. J. Med. Chem. 59, 2054–2066 (2016).
21. Nhu, D., Lessene, G., Huang, D. & Burns, C. J. Small molecules targeting Mcl-1:
the search for a silver bullet in cancer therapy. MedChemComm 7, 778–787 (2016).
22. Opferman, J. T. et al. Obligate role of anti-apoptotic MCL-1 in the survival of
hematopoietic stem cells. Science 307, 1101–1104 (2005).
23. Wang, X. et al. Deletion of MCL-1 causes lethal cardiac failure and
mitochondrial dysfunction. Genes Dev . 27, 1351–1364 (2013).
24. Thomas, R. L. et al. Loss of MCL-1 leads to impaired autophagy and rapid
development of heart failure. Genes Dev . 27, 1365–1377 (2013).
25. Lessene, G., Czabotar, P . E. & Colman, P . M. BCL-2 family antagonists for cancer
therapy. Nat. Rev. Drug Discov . 7, 989–1000 (2008).
26. Bruncko, M. et al. Structure-guided design of a series of MCL-1 inhibitors with
high affinity and selectivity. J. Med. Chem. 58, 2180–2194 (2015).
27. Tunquist, B. J., Woessner, R. D. & Walker, D. H. Mcl-1 stability determines
mitotic cell fate of human multiple myeloma tumor cells treated with the kinesin spindle protein inhibitor ARRY-520. Mol. Cancer Ther. 9, 2046–2056 (2010).
28. Oltersdorf, T. et al. An inhibitor of Bcl-2 family proteins induces regression of
solid tumours. Nature 435, 677–681 (2005).
29. Souers, A. J. et al. ABT-199, a potent and selective BCL-2 inhibitor, achieves
antitumor activity while sparing platelets. Nat. Med . 19, 202–208 (2013).30. Aubrey, B. J. et al. An inducible lentiviral guide RNA platform enables the
identification of tumor-essential genes and tumor-promoting mutations in vivo. Cell Reports 10, 1422–1432 (2015).
31. Derenne, S. et al. Antisense strategy shows that Mcl-1 rather than Bcl-2 or
Bcl-x(L) is an essential survival protein of human myeloma cells. Blood 100, 194–199 (2002).
32. Zhang, B., Gojo, I. & Fenton, R. G. Myeloid cell factor-1 is a critical survival factor
for multiple myeloma. Blood 99, 1885–1893 (2002).
33. Lee, E. F. et al. A novel BH3 ligand that selectively targets Mcl-1 reveals that
apoptosis can proceed without Mcl-1 degradation. J. Cell Biol . 180, 341–355 (2008).
34. Chen, L. et al. Differential targeting of prosurvival Bcl-2 proteins by their
BH3-only ligands allows complementary apoptotic function. Mol. Cell 17, 393–403 (2005).
35. Touzeau, C. et al. The Bcl-2 specific BH3 mimetic ABT-199: a promising
targeted therapy for t(11;14) multiple myeloma. Leukemia 28, 210–212 (2014).
36. Lazareth, A. et al. MB4-2 breakpoint in MMSET combined with del(17p)
defines a subset of t(4;14) multiple myeloma with very poor prognosis. Haematologica 100, e471–e474 (2015).
37. Zhang, H. et al. Mcl-1 is critical for survival in a subgroup of non-small-cell lung
cancer cell lines. Oncogene 30, 1963–1968 (2011).
38. Xiao, Y. et al. MCL-1 Is a key determinant of breast cancer cell survival:
validation of MCL-1 dependency utilizing a highly selective small molecule inhibitor. Mol. Cancer Ther. 14, 1837–1847 (2015).
LSKs in BM
T cells in thymus
0.1
110100Myeloid cells in BM
T cells in spleen
0.1
110Myeloid cells in spleen
B cells in BM
DN thymocytes in thymus B cells in spleen L S K s
L S K s
C e l l n u m b e r × 106
M
o n o /M
a c r o
N
e u t
r o p
h i l s
C
D 4 S
P
C
D 8 S P C D 4/C D 8 D P
C
D 4 S P
C
D 8 S P
M
o n o /M
a c r o
N
e u t
r o p h
i l s
D N
1
D N
2
D N
3
D N
4
P r e /p r
o B c e l l s S l g + B c e l l s
B 200p o s S l
g + m a t u r e B c e l l s T r a n s i t i o n a l I g M h /I g D o F o l l i c u l a r
I g M p o s –
–
+
+
–
+
–
+–
+
–+–+–+
–
+–+–+–+
–+–+–+–+
–
+
–
+
–
+
C e l l n u m b e r × 106
C e l l n u m b e r × 106
C e l l n u m b e r × 106
C e l l n u m b e r × 106
C e l l n u m b e r × 106
C e l l n u m b e r × 106
C e l l n u m b e r × 106
Figure 5 | S63845 is well tolerated in mice at doses that efficiently kill tumour cells. Cell counts of major lymphoid and myeloid subsets in the bone marrow (BM), spleen and thymus of C57BL/6–LY5.1+ mice at day 9 following treatment with 25 mg per kg body weight S63845 for 5 days (days 1–5); n = 6 vehicle and n = 6 drug treated mice (see source data). Students unpaired t-test was carried out and significant changes are
shown. LSKs, lineage marker negative, SCA1+, cKIT + haematopoietic stem cell population; SPs, CD4+, CD8? or CD4?, CD8+ single positive thymocytes; DN, CD4?CD8? double negative thymocyte progenitors; mono, monocytes; macro, macrophages; slg +, surface immunoglobulin positive.
39. Cragg, M. S., Harris, C., Strasser, A. & Scott, C. L. Unleashing the power of
inhibitors of oncogenic kinases through BH3 mimetics. Nat. Rev. Cancer9,
321–326 (2009).
40. Cragg, M. S. et al. Treatment of B-RAF mutant human tumor cells with a MEK
inhibitor requires Bim and is enhanced by a BH3 mimetic. J. Clin. Invest.118, 3651–3659 (2008).
41. Corcoran, R. B. et al. Synthetic lethal interaction of combined BCL-X L and MEK
inhibition promotes tumor regressions in KRAS mutant cancer models. Cancer Cell23, 121–128 (2013).
42. Perciavalle, R. M. et al. Anti-apoptotic MCL-1 localizes to the mitochondrial
matrix and couples mitochondrial fusion to respiration. Nat. Cell Biol. 14,
575–583 (2012).
Supplementary Information is available in the online version of the paper. Acknowledgements We thank S. Courtade-Gaiani and D. Valour for bioinformatics support, E. Borges for assistance on manuscript formatting, E. Schneider and C. Wagner-Legrand, H. Johnson, G. Siciliano and K. Hughes for technical help for in vivo studies, N. Whitehead for protein production support, P. Bouillet and L. A. O’Reilly for assistance with histology, M. Fallowfield,
J. D’Alessandro, L. T erry, V. Lemesre, J.-P. Galizzi and C. de la Moureyre for in vitro assay support, H. Simmonite for analytical support and L. Andrieu, L. Montane and A. Schmutz for biostatistical support. Research at WEHI is supported
by the National Health and Medical Research Council Australia (NHMRC,
GNT1016647, GNT1016701, GNT1020363, GNT1086291, GNT1049720, GNT1057742, GNT1079560), the Leukemia and Lymphoma Society (SCOR grant 7001-03), The Cancer Council (1086157 GLK, grant in aid to A.W.R. and D.C.S.H.), The Kay Kendall Leukemia Fund Intermediate Fellowship (KKL331 to G.L.K.), the Victoria Cancer Agency, the Australian Cancer Research Foundation, a Victorian State Government Operational Infrastructure Support (OIS) grant and the estate of Anthony (T oni) Redstone OAM.
Author Contributions A.K., Z.S., J.D., M.Cs., A.Pa., Z.B.S., S.S., G.R., A.Pr., B.B., L.O., G.B. and C.G. supervised and performed the chemistry. A.K., Z.B.S., J.M., J.D. and I.C. performed the drug design and molecular modelling. A.L.M.,
G.L.T.-B., G.L.K., J.-N.G., D.M.M., A.Stu., D.S., C.D.R., G.P., C.C., G.G. and N.C. performed cell based experiments. G.L.K., G.L.-A., A.-M.G., F.G., M.S.B.,
L.C.A.G. and M.J.H. performed the in vivo experiments. B.J.A. contributed
to the histology analysis. J.M., A.R., A.Su., P.D., N.M., J.S. and C.P. produced recombinant proteins, performed biochemical assays and crystallographic studies. M.Ch., G.L.K., A.B. and M.J.H. designed the in vivo experiments. F.M., N.G.-S. and B.L. designed and performed the bioinformatic analysis.
A.-L.M., J.M., J.D., G.L.K., F.C., J.A.H., A.W.R., D.C.S.H., A.H.W., A.Str., G.L. and O.G. supervised the studies, designed the experiments and interpreted the results.
A.Str., G.L., D.C.S.H. and O.G. wrote the manuscript with the assistance of A.L.M., G.L.K. and the other authors.
Author Information Reprints and permissions information is available at https://www.doczj.com/doc/d65421987.html,/reprints. The authors declare competing financial interests: details are available in the online version of the paper. Readers are welcome to comment on the online version of the paper. Correspondence and requests for materials should be addressed to O.G. (olivier.geneste@https://www.doczj.com/doc/d65421987.html,). Reviewer Information Nature thanks S. Fletcher, F. Stegmeier, G. Wagner and the other anonymous reviewer(s) for their contribution to the peer review of this work.
6|N A T U R E|V O L000|00M O N T H2016
over the protein surface. All sample measurements were performed at a flow rate of 30 μ l per min (injection time 120 s, dissociation time 360 s). The sensor surface was regenerated by consecutive injections of 0.35 M EDTA pH 8.0 with 0.1 mg/ml ?1 trypsin, 0.5 M imidazole and 45% DMSO (60 s, 15 μ l per min). Data p rocessing was performed using BIAevaluation 2.1 (BIAcore GE Healthcare Bio-Sciences Corp) software. Sensorgrams were double referenced before global fitting of the concen-tration series to a 1:1 binding model.
Affinity determination by competition in solution. Affinity determination by competition in solution experiments were performed at 30 °C in 10 mM HEPES pH 7.4, 150 mM NaCl, 3 mM EDTA, 1 mM TCEP , 2% glycerol, 0.05% P20 and 1% DMSO (buffer C). An MCL1-specific compound was immobilized on Series S CM5 chips by amine coupling as advised in the BIAcore GE Healthcare protocol. Serial dilutions of compounds in buffer B supplemented with fixed concentrations of protein were injected over the generated surface at a flow rate of 15 μl per min for 90 s. Calibration curves were generated using the same procedure by injecting different concentrations of protein over the same sensor chip. Affinity evaluations were performed using the affinity in solution model of BIA evaluation 2.1 (BIAcore GE Healthcare Bio-Sciences Corp) software.
Animals and treatment groups. Mice were kept in either the Servier Research Institute or the Walter and Eliza Hall Institute (WEHI) specified pathogen-free animal areas for mouse experimental purpose (for Servier, facility license number B78-100-2). The care and use of animals was in accordance with European and national regulations for the protection of vertebrate animals used for experimental and other scientific purposes (directives 86/609 and 2003/65) and the requirements of the Servier Research Institute and WEHI Animal Ethics Committees. Sample sizes were chosen to reach statistical significance, and tumour measurements and all data analysis were performed in a blinded fashion. The E μ -Myc transgenic mice
are kept on a C57BL/6–Ly5.2+
background and have been described previously 51.8–10 week old female SCID mice (for transplantation with human AMO1 and H929 tumour cells) or Swiss Nude mice (Crl:NU(Ico)-Foxn1nu) (for transplanta-tion with human MV4-11 tumour cells) were inoculated with 0.1 ml containing 5 ×106 of the indicated tumour cells subcutaneously into the right flank. The H929 and MV4-11 cells were resuspended in 100% matrigel (BD Biosciences) and the AMO1 cells in a 50:50 mixture of growth medium and matrigel. The width and length of the tumours were measured 2–3 times a week using an electronic caliper. Tumour volume was calculated using the formula: (length ×width 2)/2. When the tumour volume reached approximately 200 mm 3, mice were randomized into d ifferent groups; that is, treatment with drug (different concentrations) or vehicle (n = 8 for each group). S63845 was formulated extemporaneously in 25 mM HCl, 20% 2-hydroxy propyl β -cyclo dextrin 20% (Fisher Scientifics) and administrated
at the doses and schedules described in the figure legends. Tumour growth i nhibition (TGI max ) was calculated at the greatest response using the following
equation: –––×1100x x (median of treated at day median of treated at day 0)
(median of control at day median of control at day 0)
where day x is the day maximum where the number of animals per group in the control group is sufficient to calculate the TGI (%). For the statistical analysis of differences in tumour volume between treatment groups, a two-way ANOV A with repeated measures on day factor was performed on log-transformed data
f ollowed by Dunnett adjustment in order to compare each dose of dru
g to the control group. A complete tumour regression response was considered for the population wit
h tumours 25 mm 3 for at least three consecutive measurements. For ethical reasons, mice carrying tumours exceeding 2,000 mm 3 were euthanized. Data are represented as mean of tumour volume ± s.e.m. over time (days) until at least one mouse per cohort had to be killed.
Single-cell suspensions of 106 E μ-Myc lymphoma cell lines (AH15A, AF47A, BRE966, 2253, MRE 721, 560), resuspended in phosphate-buffered saline (PBS), were injected into the tail vein of 8–9 week old female C57BL/6–Ly5.1+ mice. Mice were treated with either vehicle (25 mM HCl, 20% 2-hydroxy propyl β -cyclo d extrin) or 25 mg kg ?1 S63845 (reconstituted in vehicle) on days 5–9 after
t ransplant, administered by tail vein injection or, in some incidences when the tails became damaged, by retro-orbital injection. To generate the survival curves of the mice bearing the E μ-Myc lymphoma cells, mice were killed when deemed unwell by experienced animal technicians. For the toxicity experiments, female C57BL/6–Ly5.1+ mice bearing E μ-Myc lymphomas or non-tumour bearing C57BL/6–Ly5.1+ mice were killed 4 days after the 5-day drug treatment regimen had been c ompleted (this equated to 13 days after transplantation of the tumour cells in the mice b earing the E μ-Myc lymphoma cells). For the three mice injected
with the AH15A E μ-Myc lymphoma cells, those treated with vehicle were a nalysed
after only 4 days of treatment because they were deemed too unhealty from the lymphoma to complete their prescribed regimen. For the maximal tolerated dose experiments, 7–8 week old C57BL/6 mice (3 male and 3 female mice in each arm) were treated with a dose of vehicle or S63845 (25 mg per kg, 40 mg per kg, 50 mg
METHODS
Compounds. Lapatinib, PLX-4032, trametenib, tarceva, ABT-199 and ABT-263 were purchased from Selleck-chem; QVD-OPh from Sigma; MG132 from Calbiochem; idarubicin and araC from Pharmacia and Upjohn. A-1210477 was made according to published methods 26. Synthesis and characterization of S63845 is provided in the Supplementary Methods. Owing to light sensitivity, S63845 was stored in the dark.
MCL1 protein expression and purification. Following the previously published structure of MCL1 (PDB ID4WGI)43, a construct was designed with residues 173–321 of human MCL1 as a C-terminal fusion with maltose binding protein (MBP). In addition to the surface entropy-reducing (SER) mutations in MCL1 (K194A, K197A and R201A (ref. 43)), we also introduced E198A, E199A and K265A mutations into MBP (ref. 44).
The plasmid encoding the MBP–MCL1 fusion protein was transformed into BL21(DE3)pLysS bacteria. A single colony was used to inoculate 5 ml terrific broth (Fisher BioReagents, (BP2468-2)) containing kanamycin and chloramphenicol at 100 μg ml ?1 and 34 μg ml ?1, respectively. After 3 h growth at 37 °C, the 5 ml culture was used to inoculate 2 l terrific broth containing the same antibiotics. At an OD 600 of 0.7, the temperature was reduced to 18 °C before induction of MBP–MCL1 protein expression by addition of IPTG to a final concentration of 1 mM. Cells were harvested by centrifugation.
Harvested cells were resuspended in 3 volumes of 20 mM Tris–HCl pH 7.4, 200 mM NaCl, 2 mM EDTA, 1 mM DTT and lysed by passing three times through an emulsiflex-C5 (Avestin). The lysate was clarified by centrifugation at 40,000 g , at 4 °C, for 60 min and applied to a 5-ml MBPTrap column (GE Healthcare). The MBP–MCL1 fusion protein was eluted in 20 mM Tris-HCl pH 7.4, 200 mM NaCl, 2 mM EDTA, 1 mM DTT, 10 mM maltose and further purified by size exclusion chromatography in 20 mM HEPES, 100 mM NaCl and 1 mM DTT. Protein eluted as a monomer was concentrated and used in crystallization studies.
Crystallization studies. Apo crystals were grown at a concentration of 34 mg ml ?1 (20 mM HEPES pH 7.5, 150 mM NaCl and 2 mM DTT) by the sitting drop vapour diffusion. 2 μ l of the protein solution was mixed with 2 μ l of the crystallization reservoir (25% PEG 3350, 0.2 M magnesium formate, 1 mM maltose) in a sitting drop plate. The plate was incubated at 284 K and suitable rod-like crystals appeared overnight. Individual crystals were harvested from the crystallization drops and transferred to a drop containing 4.5 μ l of the crystallization reservoir solution plus 0.5 μ l of S63845 (20 mM in DMSO). The mixture was incubated for 72 h at 284 K. Crystals were flash frozen in liquid nitrogen after cryoprotection using crystalli-zation reservoir plus 20% ethylene glycol.
Structure solution. Diffraction data were collected at the Soleil Synchrotron (France) on a beamline Proxima1 and were processed and scaled using XDS (ref. 45). The structure was solved by molecular replacement using MOLREP (ref. 46), using another crystal structure of an MBP–MCL1 fusion protein 43. The data were subsequently refined using REFMAC5 (ref. 47). Interactive graphical model building was carried out with COOT. The ligand was clearly defined by the initial electron density maps. The progress of the refinement was assessed using R free and the conventional R factor. Once refinement was completed, the structures were validated using various programs from the CCP4i package, CCP4. Statistic parameters are detailed in Extended Table 1.
Fluorescence polarization. Fluorescence polarization assays were carried out in black-walled, flat-bottomed, low-binding, 384-well plates (Corning) in buffer A (10 mM HEPES, 150 mM NaCl, 0.05% Tween 20 pH 7.4 and 5% DMSO) in the presence of 10 nM fluorescein-PUMA (3-(((3′,6′-dihydroxy-3-oxo-3H-spiro(2-benzofuran-1,9′-xanthene)-5-yl)carbamothioyl)amino)-N -(6-oxohexyl) propanamide-AREIGAQLRRMADDLNAQY, from the polypeptide group, France). Final concentrations of MCL1, BCL-2 and BCL-X L proteins were 10, 10 and 20 nM, respectively. The assay plates were incubated for 2 h at room t emperature and the fluorescence polarization was measured on a Synergy 2 reader (exitation, 528 nm; emission, 640 nm; cut-off, 510 nm). The binding of increasing doses of the compound was expressed as a percentage reduction in mP compared to the window established between the ‘DMSO only’ and ‘total inhibition’ c ontrol (30 μ M PUMA). The inhibitory concentrations of the drugs that gave a 50% r eduction in mP (IC 50) were determined, from 11-point dose response curves, in XL-Fit using a 4-parameter logistic model (Sigmoidal dose–response model). The K i was subsequently calculated as described in ref. 48.
Surface plasmon resonance. All SPR measurements were performed on a BIAcore T200 instrument (BIAcore GE Healthcare).
Direct binding assay. Direct binding experiments were performed at 20 °C on Series S NTA chips. 10 mM HEPES pH 7.4, 175 mM NaCl, 25 μ M EDTA, 1 mM TCEP , 0.01% P20 and 1% DMSO was used as a running buffer (buffer B). The ligand surface was generated using double His-tagged proteins essentially as described in refs 49, 50. Serial dilutions of the compound in buffer B were injected
per kg or 60 mg per kg body weight) for 5 consecutive days by i.v. tail vein i njection or by retro-orbital injection if the tails became damaged. The mice were analysed as they were killed, or for the mice surviving the entire course of treatment, 3 days after the 5-day treatment had been completed. For the initial toxicity studies, sections of spleen, lymph nodes, thymus, ovaries, uterus, kidneys, liver, pancreas, intestines, colon, heart, lung, sternum, backbone and muscle were fixed in 10% formalin and stained with haematoxylin and eosin. The weights of the spleen, thymus, (axillary, brachial and inguinal) lymph nodes, liver and kidneys were recorded. Cells were flushed from the bone marrow (two femurs and one tibia) and single cell suspensions of the spleen, thymus and lymph nodes were generated. The red blood cells were lysed by treatment with 0.168 M ammonium chloride and the white blood cell count was determined using a CASY cell counter (Scharfe System GmbH).
Primary AML patient samples. All bone marrow or peripheral blood samples from patients with AML were collected after informed consent in accordance with guidelines approved by the Alfred and Royal Melbourne Hospital human research ethics committees. Mononuclear cells were isolated by Ficoll-Paque (GE Healthcare) density-gradient centrifugation, followed by red cell depletion in ammonium chloride (NH4Cl) lysis buffer at 37 °C for 10 min. Cells were then resuspended in PBS containing 2% fetal bovine serum (FBS, Sigma). Mononuclear cells were suspended in RPMI-1640 (Gibco) medium containing penicillin and streptomycin (Gibco) and 15% heat-inactivated FBS (Sigma). Normal CD34+ progenitor cells from healthy donors were collected from granulocyte colony stimulating factor (G-CSF)-mobilized blood harvests and purified after Ficoll separation by CD34 positive selection using Miltenyi Biotec micobeads (Miltenyi Biotec. Cat. No. 130-046-703).
Human research ethics approval. The research with primary human cells was approved by the Human Research Ethics Committee (HREC) of Alfred Health. AML cells from patients and cells from normal donors were obtained f ollowing informed consent processes approved by the HRECs of Alfred Health and Melbourne Health.
Agar colony formation assays. Colony-forming assays were performed on freshly purified and frozen mononuclear fractions from AML patients or normal cells from G-CSF mobilized normal, healthy donors. Primary cells were cultured in duplicate in 35-mm dishes (Griener-bio) at 104 to 105 cells. Cells were plated in 0.6% agar (Difco): AIMDM 2×(IMDM powder, Invitrogen), supplemented with NaHCO3, dextran, penicillin and streptomycin, β-mercaptoethanol and asparagine, FBS (Sigma) at a 2:1:1 ratio of agar:AIMDM:FBS. For optimal growth conditions, all plates contained granulocyte/macrophage colony stimulating factor (100 ng per plate, genzyme), IL-3 (100 ng per plate, R&D Systems), stem cell factor (100 ng per plate, R&D Systems) and erythropoietin (4U per plate, Roche). Cells were cultured for 2–3 weeks in the presence or absence of drugs at 37 °C at 5% CO2 in a high humidity incubator. After incubation, plates were fixed with 2.5% glutaraldehyde in saline and scored using GelCount (Oxford Optronix).
Cell culture. NCI-H929, RS4;11, MV4-11, HCT-116, BT-474, SK-Mel-2, PC-9 and H146 cells were cultured in RPMI 1640 medium, A2058 cells were cultured in DMEM medium and SK-MEL-28 cells were cultured in EMEM medium. All media were supplemented with 10% heat-inactivated FBS, 2 mM l-glutamine, 100 U ml?1 penicillin, 100 μg ml?1 streptomycin, and 10 mM HEPES pH =7.4, at 37 °C, in 5% CO2. For RS4;11 cells the medium was additionally supplemented with 4.5 g l?1 glucose. AMO1 cells were cultured in RPMI 1640 medium supplemented with 20% heat-inactivated FBS, 2 mM l-glutamine, 100 U ml?1 penicillin, 100 μg ml?1 streptomycin, and 10mM HEPES pH =7.4. HeLa cells were cultured in DMEM medium (containing 10% heat-inactivated FBS, 10 mM HEPES, 100 U ml?1 penicillin, 100 μg ml?1 streptomycin). Cells were grown at 37 °C in a humidified atmosphere with 5% CO2. All of the cell lines were purchased from the ATCC or DSMZ.
Human Burkitt lymphoma (BL)-derived cell lines (Rael-BL, Kem-BL, BL2, BL30, BL31, BL41, and Ramos-BL, a gift from A.B. Rickinson and M. Rowe, University of Birmingham, UK) were cultured in RPMI 1640 medium s upplemented with 10% heat-inactivated FBS, 1 mM glutamine, 1 mM sodium pyruvate, 50 μM α-t hiogycerol (Sigma), and 20 nM bathocuproine disulfonic acid (Sigma) in a humidified incubator at 37 °C, 5% CO2. The mouse Eμ-Myc lymphoma cell lines (AH15A, AF47A, 2253, BRE966, MRE 721 and 560) were cultured in high-glucose DMEM supplemented with 10% heat-inactivated FBS, 50 μMβ-m ercaptoethanol (Sigma), 100 μM asparagine (Sigma), 100 U ml?1 penicillin and 100 mg ml?1 streptomycin in a humidified incubator at 37 °C, 10% CO2.
The myeloma-derived cell lines were purchased from the ATCC, DSMZ or JCRB or provided by the laboratory of A. Spencer (XG1, KMS-26, ANBL6, WL-2 and OCI-MY1) and cultured as recommended by the suppliers at 37 °C in the presence of 5% CO2. Bax?/?,Bak?/? H929, KMS-12-PE and AMO1 cells were generated using CRISPR/Cas9 genome editing as described below. HEK293T cells were cultured in DMEM supplemented with 10% heat-inactivated FBS at 37 °C in the presence of 10% CO2. Media and supplements were purchased from Life Technologies unless specified otherwise.
To test the sensitivity of 152 cell lines derived from several types of solid tumours or haematological malignancies (AML, lymphoma, bladder, central nervous s ystem, colorectal, gastric, head and neck, liver, lung, breast, melanoma, ovarian, pancreas, prostate, renal, sarcoma and uterine) to S63845, cells were grown at 37 °C in a humidified atmosphere with 5% CO2 in RPMI 1640 medium (25 mM HEPES, with l-glutamine, Biochrom) supplemented with 10% (v/v) FBS (Sigma) and 0.1 mg ml?1 gentamicin (Life Technologies). Different culture media were used for VCap (DMEM, 10% FCS, 1% gentamycin), CALU1 (McCoy, 10% FCS 1% gentamycin) and U87MG (EMEM, 10% FCS 1% gentamycin). These cell lines were provided by the Children’s Hospital Cologne, the University Hospital Freiburg or the NCI or were purchased from ATCC, DSMZ, JCRB, ECACC or KCBL.
Two cell lines used in this study were present in the list of commonly m isidentified cell lines maintained by the International Cell Line Authentication Committee (ICLAC): NCI-H929 and U-937. For our study, H929 cells were obtained from authentic stocks (ATCC CRL-9068 and DSMZ ACC-163) and U937 cells were authenticated by STR analysis. All cell lines used in this study were v erified to be mycoplasma negative before undertaking any experiments with them. MTT cell viability assay. Cell viability was measured using MTT (3-(4,5- dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) colourimetric assay. Cells were seeded in 96-well microplates at a density to maintain control (untreated) cells in an exponential phase of growth during the entire experiment. Cells were incubated with compounds for 48 h followed by incubation with 1 mg ml?1 MTT for 4 h at 37 °C. Lysis buffer (20% SDS) was added and absorbance was m easured at 540 nm 18 h later. All experiments were repeated at least three times. The p ercentage of viable cells was calculated and averaged for each well: per cent growth =(OD treated cells/OD control cells) ×100, and the IC50, the concentration where the optical density was reduced by 50%, was calculated by a linear regression performed on the linear zone of the dose–response curve.
CellTiterBlue cell viability assay. Cells were harvested from exponential phase cultures, counted and plated in 96-well flat-bottom microtitre plates at a cell d ensity depending on the cell line’s growth rate (4,000 to 30,000 cells for solid- t umour-derived cell lines, 10,000 to 60,000 for haematological cancer-derived cell lines). After a 24-h recovery period to allow the cells to resume exponential growth, 10 μl of culture medium (four control wells per plate) or of culture medium with the test compound were added by a liquid-handling robotic system and treated or untreated cells were cultured for a further 3 days. Compounds were applied in half-log increments at 10 concentrations in duplicate. After treatment of cells, 20 μl per well CellTiter-Blue reagent (Promega) was added. After incubation for up to 4 h, fluorescence was measured by using the Enspire Multimode Reader (Perkin Elmer, excitation λ=531 nm, emission λ=615 nm). IC50 values were calculated by 4-parameter, nonlinear curve fit using Oncotest Warehouse Software. CellTiter-Glo luminescent cell viability assay. To test the activity of S63845 in combination with the kinase inhibitors trametenib, tarceva, PLX-4032 and lapatinib, SK-MEL-28, BT-474, A2058, SK-Mel-2 and PC-9 cells were seeded into 96-well plates. After 24 h, cells were treated with the indicated compounds for 72 h and assayed for viability using the CellTiter-Glo reagent (Promega). Luminescence was measured at 0, 24, 48 and 72 h on independent plates seeded and treated at the same time. Results were normalized to the samples without treatment at time 0 h. To test the sensitivity of the multiple myeloma cell lines to S63845 cells were seeded into 96-well plates at 5,000 cells per well and treated at 5-point 1:8 serial dilutions of compounds starting from 10 μM. Cell viability was assessed at 48 h using the CellTiter-Glo Assay (Promega) following the manufacturer’s instructions and the plates were read using an Envision luminescence plate reader (Perkin Elmer). Results were normalized to the viability of cells that had been treated with 0.1% DMSO (vehicle) in medium for 48 h. The IC50 values were calculated using nonlinear regression algorithms in Prism software (GraphPad).
To test the dependence of H929 cells on BCL-2, BCL-X L, BCL-W, MCL1 or A1/BFL1 for their sustained survival, pools of cells stably expressing Cas9 (mCherry+) and inducibly expressing the relevant single guide RNA (sgRNA) (GFP+) were purified by flow cytometry (BD Biosciences) and seeded into 96-well plates (5,000 cells per well) in triplicates and their viability was determined by using the CellTiter-Glo assay 72 h after the addition of doxocycline (1 μg ml?1) to induce expression of the sgRNA targeting the corresponding genes. The data were n ormalized to the viability of cells infected with the empty vector. In some e xperiments, the viability (determined by propidium iodide exclusion) of the cells with or without co-treatment with the pan-caspase inhibitor QVD-OPh (25 μM; MP Biomedicals) for 12 h was also determined.
Cell viability analysis of primary AML patient samples. Freshly purified m ononuclear cells from AML patient samples were adjusted to a concentration of
2.5 ×105 per ml1 and 100 μl of cell suspensions were aliquoted per well into 96-well plates (Sigma). Cells were then treated with S63845, cytarabine (Pfizer), ABT-199 (Active Biochem) or idarubicin (Sigma) over a 6 log concentration range from 1 nM to 10 μM for 48 h and incubated at 37 °C, 5% CO2. Cells were then stained with the Sytox blue nucleic acid stain (Invitrogen) and fluorescence measured by flow cytometric analysis using a LSR-II Fortessa machine (Becton Dickinson). FACSDiva software was used for data collection, and FlowJo software for data analysis. Blast cells were gated using forward and side light scatter properties. Viable cells excluding Sytox blue were determined at six concentrations for each drug and the 50% lethal concentration (LC50, in μM) was calculated using nonlinear regression algorithms in Prism software (GraphPad).
Cell viability analysis by Annexin V/propidium iodide staining. NCI-H929 cells were treated with the indicated compounds for 4 h, centrifuged and washed with binding buffer (10 mM HEPES, 140 mM NaCl, 2.5 mM CaCl2). Cells were incubated with 200 μl of binding buffer containing Annexin V–Alexa fluor 488 (Invitrogen) and propidium iodide (Sigma) for 15 min at 20 °C in the dark. 400 μl of binding buffer was added and samples were kept at 4 °C before flow cytometry analysis. For each sample, 104 cells were analysed by flow cytometry in an Epics XL/MCL flow cytometer (Beckman Coulter). Fluorescence was collected at 520 nm (Alexa fluor 488) and 630 nm ( propidium iodide).
Human Burkitt lymphoma-derived cell lines and mouse Eμ-Myc lymphoma cell lines were plated at a density of 4 ×104 cells per well in flat-bottomed 96-well plates. These cells were treated with increasing doses of S63845 (typically 0.008, 0.025, 0.04, 0.2, 1, 5 μM) for 24 h. Cells were stained with Annexin V-FITC and propidium iodide, analysed on a FACS Calibur and live cells (Annexin V negative/ propidium iodide negative) were recorded. Data are presented as per cent cell death induction relative to cells cultured in medium alone. Immunodetection of cleaved PARP by MesoScale discovery assay. Twenty-four hours after seeding, cells were treated with the indicated compounds for 6 h and harvested in lysis buffer (10 mM HEPES pH 7.4, 142.5 mM KCl, 5 mM MgCl2, 1 mM EDTA, 1% NP40, protease and phosphatase inhibitors cocktails (Calbiochem)). Cleared lysates (5 μg protein) were prepared for immunodetection of cleaved PARP (a marker of apoptosis) by using the MSD apoptosis panel whole cell lysate kit (MSD) in 96-well plates according to manufacturer’s instructions, and were analysed on the Sector Image 2400.
Cytochrome c release assay. NCI-H929 cells were treated with S63845 for 4 h, washed with PBS and harvested in lysis buffer delivered with the cytochrome c release apoptosis assay kit (Qiagen). Cells were then homogenized using an ice-cold tissue grinder (40 passes). Homogenates were centrifuged at 700 g for 10 min at 4 °C. The supernatants were transferred into fresh tubes and centrifuged at 10 000 g for 30 min at 4 °C. The supernatants were collected as cytosolic fractions. Cytochrome c release was determined by western blotting using the cytochrome c antibody provided in the kit. Lysates were also analysed by immunoblotting using an anti-LDH antibody (Rockland 200-1173; used as protein loading control). Immunoblotting. Total protein extracts of myeloma cells were generated in lysis buffer (20 mM Tris-HCl pH 7.4, 135 mM NaCl, 1.5 mM MgCl2, 1 mM EDTA, 10% glycerol) containing 1% Triton X-100 and complete protease inhibitors (Roche). Protein extracts of the other cell lines were generated in lysis buffer containing 10 mM HEPES pH 7.4, 142.5 mM KCl, 5 mM MgCl2, 1 mM EDTA, 1% NP40, protease and phosphatase inhibitors cocktails (Calbiochem). Lysates were stored at ?80 °C. Protein content was quantified using the Bradford assay (Bio-Rad). Lysates were diluted with LDS sample buffer (Invitrogen) at a 3:1 ratio and d enatured at 95 °C for 7–10 min. 20–40 μg of protein extracts were separated by SDS–PAGE (NuPAGE 10% Bis Tris gels) and proteins transferred onto nitrocellulose m embranes. The membranes were blocked in 5% skimmed milk in PBS and 0.1% Tween20 (blocking buffer) before incubation with antibodies. Rat m onoclonal antibodies to BAX (21C10; WEHI) or BAK (7D10; WEHI) and mouse monoclonal antibody against HSP70 (N6; used as a loading control) were used. All a ntibodies were diluted in blocking buffer. Commercially available antibodies were also used: rabbit polyclonal antibodies against MCL1 (Santa Cruz, S-19, sc-819), PARP (Cell Signaling, 9542), BIM (Cell Signaling, C34C5 2933), Phospho-ERK (Cell Signaling, 9101), total ERK (Cell Signaling, 9102), BAK (BD 556396), BAX (Santa Cruz, sc-493) BCL-X L (Transduction Laboratory, 610212) and mouse monoclonal antibodies against actin (Millipore, MAB1501R; used as a loading control), NOXA (Calbiochem, OP180), Flag-M2 (Sigma) and p53 (Santa Cruz, sc-126).
Co-immunoprecipitation. HeLa cells were transiently transfected, using the Effecten reagent (Qiagen), with expression vectors encoding 3×Flag-tagged MCL1, BCL-X L or BCL-2 (p3×F lag–CMV10, Sigma). After 24 h, cells were treated for 4 h with S63845 and then harvested in lysis buffer (10 mM HEPES pH 7.5, 150 mM KCl, 5 mM MgCl2, 1 mM EDTA, 0.4% Triton X100, protease and p hosphatase inhibitors cocktails (Calbiochem)). The cleared lysates were subjected to immunoprecipitation with anti-Flag M2 agarose beads (Sigma). The i mmunoprecipitates and inputs were analysed by immunoblotting using the a ntibodies listed above.
Analysis of MCL1 gene expression by qPCR. Total RNA was extracted using RNeasy mini kit with DNase I treatment (Qiagen) and reverse transcripted using a high-capacity cDNA reverse transcription kit with RNAse inhibitor (Life Technologies). Conventional real-time PCR was performed on an ABI 7900HT system in 50 μl reaction volumes containing 2×TaqMan universal PCR master mix, 2.5 μl of 20×target/control assay mix and 5 μl of respective cDNA in an optical 96-well plate. NTCs (no template controls) using RNase-free water were included in the plate. Cycling conditions were 95 °C (10 min), followed by 40 PCR cycles at 95 °C (15 s) and 60 °C (1 min). TaqMan Gene Expression Assays (Life Technologies) for MCL1 evaluated the anti-apoptotic long (L) isoform NM_021960 (reference assay Hs01050896_m1). Two out of five reference genes including GAPDH, PPIA, 18S, UBC and SDHA, were selected on geNorm software as the optimal number of reference target genes (geNorm pairwise variation cut off V<0.15). As such, the optimal normalization factor was calculated as the g eometric mean (GM) of reference targets SDHA and PPIA (ref genes) and c alculation of ?ΔC t was achieved as follows: –
?Δ=.
C C C
()
t t t
ref genes GM target gene Data are presented as fold change of relative quantification calculated as 2–ΔΔCt, with ΔΔ=Δ?Δ
C C C
t t t
treated control
. Pair-wise comparisons were evaluated with a t-test.
Antibodies for flow cytometry. Aliquots of cells were stained in 24G2 (anti-FcγR, (Fcγgamma receptor)) antibody containing hybridoma supernatant, c ontaining fluorescently (FITC, R-PE or APC) labelled monoclonal antibodies against cell surface markers, and analysed on an LSR11C (Becton Dickinson) excluding p ropidium iodide +(dead) cells. The following antibodies were used: anti-CD25 (clone PC61), anti-CD4 (clones GK1.5 (Biolegend) and H129), anti-CD8 (clones 53-6.7 (Biolegend) and YTS 169), CD44 (clone IM7), anti-B220 (220 kDa form of CD45 expressed on B cells, clones RA3-6B2 (Biolegend)), anti-GR1 (granulocyte antigen 1, clone RB6-8C5), anti-MAC1 macrophage antigen 1, clone M1/70), anti-SCA1 (stem cell antigen 1, clone E13-161.7), anti-c-KIT (clone 2B8 (Biolegend)), anti-TCR (T cell receptor, Biolegend), anti-TER119 (clone TER-119), anti-IgM (clone 5.1), anti-IgD (clone 11-26C), anti-Ly5.1 (clone A20.1) and anti-Ly5.2 (clone S.450-15.2). Data were processed using FlowJo Version 9.9 (TreeStar).
Blood analysis. Blood cell counts and cell subset composition were determined using an ADVIA 2120 haematology analyser (Siemens).
Plasmids, lentivirus production and infection. The vectors for the constitu-tive expression of Cas9 and the inducible expression of the sgRNAs have been previously described30. To target the BCL-2 family members, sgRNAs were designed (https://www.doczj.com/doc/d65421987.html,) and cloned into pFH1tUTG (ref. 30) with the exception of sgRNAs for MCL1, which have been previously described30. The sequences of the sgRNAs used in this study as well as the primers for amplifying the t argeted regions for DNA sequence analysis are detailed in Supplementary Tables 1 and 2, r espectively. The vectors to express the BIM variants have been previously described12,13. To produce lentiviruses, the constructs of interest were co- t ransfected into HEK293T cells with the packaging viruses pMDLg/pRRE, pRSV RRE and pCMV VSV-G (all from Addgene) using the Effectene t ransfection r eagent (Qiagen). The lentiviruses were harvested, filtered and used to infect target cells as previously described13,30.
CRISPR/Cas9 genome editing. Multiple-myeloma-derived cell lines were serially infected with lentiviruses that stably co-express Cas9 and the fluorescent marker, mCherry, and inducibly express the indicated sgRNAs plus stably express GFP. Double positive cells (mCherry+ GFP+) were purified using a BD FACSAria Fusion Sorter (BD Biosciences). Expression of the sgRNA was induced by the addition of doxycycline (1 μg ml?1; Sigma). The experiments targeting BCL-2, BCL-X L, BCL-W, MCL1 and BFL1 were undertaken with pools of infected cells. To generate the BAX?/?,BAK?/? H929 clone, a BAX-deficient H929 clone was infected with a lentivirus expressing a sgRNA to target BAK, re-cloned and verified by DNA sequencing and western blotting (Fig. 2c). Sequences of sgRNAs and primers for targeted PCR used in this study are shown in Supplementary Tables 1 and 2. DNA sequence verification was carried out as previously described30. Briefly, genomic DNA was isolated using the DNeasy kit (Qiagen) and mutation of targeted DNA confirmed by the Illumina MiSeq30. The unique PCR primers with overhang sequences for each sgRNA are listed in Supplementary Table 2.
Statistical analysis. Graphpad Prism software was used for generating Kaplan–Meier animal survival plots of vehicle and S63845 treated mice and performing statistical analysis (using a log-rank test (Mantel–Cox)). Graphpad Prism was also used to perform multiple unpaired two-tailed t-tests of vehicle-treated and S63845-treated mice to look for significant changes in the data generated from the ADVIA analysis of the blood and from the FACS analysis of the number of different cells present in the spleen, thymus, lymph nodes and bone marrow. Graphpad Prism was used to generate IC50 curves for cell lines treated with S63845 in vitro. GraphPad
Software was used for statistical analysis. All data are expressed as mean ±s.d. P<0.05 was considered to be significant.
Data availability. The PDB deposition code for the X-ray structure of the MBP-MCL1 complex with S63845 is 5LOF.
43. Fang, C. et al. Single diastereomer of a macrolactam core binds specifically to
myeloid cell leukemia 1 (MCL1). ACS Med. Chem. Lett.5, 1308–1312
(2014).
44. Moon, A. F., Mueller, G. A., Zhong, X. & Pedersen, L. C. A synergistic approach to
protein crystallization: combination of a fixed-arm carrier with surface entropy reduction. Protein Sci. 19, 901–913 (2010).
45. Kabsch, W. XDS. Acta Crystallogr. D Biol. Crystallogr. 66, 125–132 (2010).
46. Vagin, A. & Teplyakov, A. MOLREP: an automated program for molecular
replacement. J. Appl. Cryst.30, 1022–1025 (1997).47. Murshudov, G. N., Vagin, A. A. & Dodson, E. J. Refinement of macromolecular
structures by the maximum-likelihood method. Acta Crystallogr. D Biol.
Crystallogr. 53, 240–255 (1997).
48. Nikolovska-Coleska, Z. et al. Development and optimization of a binding assay
for the XIAP BIR3 domain using fluorescence polarization. Anal. Biochem.332, 261–273 (2004).
49. Murray, J. B., Roughley, S. D., Matassova, N. & Brough, P. A. Off-rate screening
(ORS) by surface plasmon resonance. An efficient method to kinetically
sample hit to lead chemical space from unpurified reaction products. J. Med.
Chem.57, 2845–2850 (2014).
50. Meiby, E. et al. Fragment screening by weak affinity chromatography:
comparison with established techniques for screening against HSP90.
Anal. Chem.85, 6756–6766 (2013).
51. Adams, J. M. et al. The c-myc oncogene driven by immunoglobulin enhancers
induces lymphoid malignancy in transgenic mice. Nature318, 533–538 (1985).
Extended Data Figure 1 | Biophysical characterization of the binding of MCL1 inhibitors to human and mouse MCL1 and serum effect on their cellular potency. a, Affinity comparison of binding of S63845 to human or mouse MCL1 (n=4 and 3 biological replicates for human and mouse, respectively; see source data). b, Binding affinity data of S63845 and
A-1210477 for MCL1 (fluorescence polarization (FP) and SPR), BCL-2 (fluorescence polarization) and BCL-X L (n=2 for fluorescence polarization and n=3–4 for SPR, see source data). c, SPR sensograms,
K D and kinetic parameters for the binding of S63845 and A-1210477 to human MCL1 (n=4 and 3 biological replicates for S63845 and A-1210477, respectively). d, Impact of serum concentration (FBS, fetal bovine serum) on the biological activity of the MCL1 inhibitors, S63845 and A-1210477, in H929 cells (n=
3 biological replicates, see source data).
Extended Data Figure 2 | Targeting MCL1 genetically in H929 cells induces caspase-mediated cell death. a, H929 cells rely on MCL1 for their survival. The viability of H929 cells was determined with CellTiter-Glo assays 72 h after addition of doxocycline to induce expression of sgRNAs to target BCL-2, BCL-X L, BCL-W, MCL1 or BFL1 using CRISPR/ Cas9 technology30. Two sgRNAs were tested for each gene: sg#1 (no fill pattern) and sg#2 (slash pattern). Mean and individual data points of
n=2 biological replicates performed in triplicate are shown (see source data). b, Targeting MCL1 by CRISPR/Cas9 causes rapid cell death. The viability (CellTiter-Glo assays) of H929 cells stably expressing Cas9 and containing an inducible expression construct for a sgRNA to target MCL1was determined 0–96 h after addition of doxocycline. Mean and individual data points of at least n=2 biological repicates performed in triplicate are shown (see source data). c, Caspases mediate the killing of H929 cells when MCL1 is genetically targeted. The viability (propidium iodide uptake determined by flow cytometry) of H929 cells after switching on the expression of the indicated sgRNAs by the addition of doxocycline (+D OX) was measured after culture in the presence (+) or absence (?) of the broad-spectrum caspase inhibitor, QVD-OPh (25 μM).Data (mean ±s.d.) are derived from one experiment performed in triplicate (see source data). EV
, empty vector.
Extended Data Figure 3 | Impact of treatment with S63845 on the interaction of MCL1 with pro-apoptotic BCL-2 family members
and on the level and stability of MCL1. a, HeLa cells transduced
with Flag–BCL-X L, Flag–BCL-2 or Flag–MCL1 expression constructs were treated for 4 h with increasing concentrations of S63845, before immunopreciptation using anti-FLAG antibody. Immunoprecipitates and total inputs were analysed by immunoblotting for the FLAG-tagged proteins as well as the associated BAK and BAX proteins. For gel source images, see Supplementary Fig. 1. b, HCT-116 cells were incubated for 16 h with increasing concentrations of the proteasome inhibitor, MG132, as a control, before assessing the levels of MCL1, BCL-X L and actin (protein loading control) by immunoblotting. c, HCT-116 cells were pre-incubated for 1 h with DMSO or 1 μM S63845 and then treated with the translation inhibitor, emetin (20 μg ml?1), for 0.5, 1, 2 or 4 h. Determination of MCL1 protein levels was performed by immunoblotting (actin served as a loading control). d, Densitometry of MCL1 immunoblot (Extended Data Fig. 3c, long exposure for DMSO-treated cells and short exposure for S63845-treated cells) and MCL1 half-life estimation (21 min for DMSO-treated cells and 79 min for S63845-treated cells). e, HCT-116 cells were incubated for 16 h with 300 nM S63845, or transfected with 3×Flag–MCL1 expressing plasmid (400 ng, for 48 h) before assessing MCL1 mRNA level
by reverse transcriptase–PCR quantification (see source data).
Extended Data Figure 4 | S63845 induces apoptosis of sensitive tumour derived cell lines. a, PARP cleavage in H929 cells after treatment for 6 h with the MCL1 inhibitors, S63845 or A-1210477. Mean and individual data points from three biological replicates are shown (see source data). b, Treatment with S63845 causes mitochondrial release of cytochrome
c in sensitive cells. H929 cells were incubate
d for 4 h with increasing concentrations of S63845 befor
e assessing cytochrome c abundance in the cytosolic fraction by immunoblotting. LDH was used as a protein loading control. For gel source images, see Supplementary Fig. 1. c, Treatment with MCL1 inhibitors causes PARP cleavage in sensitive cells. AMO1 and MV4-11 cells were treated for 6 h with increasing concentrations o
f the MCL1 inhibitors, S63845 or A-1210477. Cleaved PARP
(a marker of apoptotic cell death) was detected by a Meso Scale eletrochemiluminescence assay. Means and individual data points from
three biological replicates are shown (see source data).
Extended Data Figure 5 | Correlation between the sensitivity of multiple-myeloma-derived cell lines to S63845 and killing by the MCL1-selective ligand BIM2A. BAX/BAK dependency for S63845-induced killing in KMS-12-PE and AMO1 myeloma cells. Expression of pro-survival BCL-2 family proteins across a panel of multiple-myeloma-derived lines. a , Correlation between the sensitivity of multiple myeloma (MM)-derived cell lines to S63845 and killing by enforced expression of the MCL1-selective ligand BIM2A. The sensitivity of 25 multiple-myeloma-derived cell lines to S63845 was plotted against the viability of the same cells infected with a lentivirus that expresses the MCL1-selective ligand BIM2A (ref. 33) (r = 0.55) or with a lentivirus expressing the BCL-2, BCL-X L and BCL-W binding ligand BIM–BAD (ref. 34) (r =? 0.22) (data from Extended Fig. 5b, see source data). The r and P values were determined by Pearson correlation analysis.
b , Table of IC 50 values and per cent viability as defined in Extended Data Fig. 5a measured using the CellTiter-Glo assay. The IC 50 values were calculated from 2–5 biological replicates (see source data, mean ±s.d.).As a comparison, the dependence of these multiple myeloma cell lines on MCL1 or BCL-2/BCL-X L /BCL-W was validated by a geneti
c approach. The survival of multiple myeloma cell lines 24 h after enforce
d expression of BIM2A (which inhibits MCL1) or BIM–BAD (which inhibits BCL-2,
BCL-X L and BCL-W) was determined by CellTiter-Glo assay and data were normalized to the survival observed when the inert BIM variant (BIM4E) was expressed. These BIM variants have been previously described 13,34; the data with the BIM variants, shown for comparison, are extracted from a larger data set 17. The multiple myeloma cell lines are grouped based on their characteristic cytogenetic abnormality. c , BAX/BAK-dependent killing of KMS-12-PE and AMO1 myeloma cells by
S63845. KMS-12-PE or AMO1 myeloma cells were engineered to lack BAX and BAK using CRISPR/Cas9 technology 1 (see Methods). Cells expressing the sgRNA empty vector (sgEV) were also generated to serve as negative controls. These cells were treated with S63845 and their viability was
determined after 48 h by the propidium iodide exclusion assay. Data shown are mean viability ± s.d. derived from three (KMS-12-PE) or two (AMO1) biological replicates (see source data). d , Expression of MCL1 and related pro-survival BCL-2 proteins across a selected panel of multiple-myeloma-derived lines (shown in Fig. 2a). The levels of MCL1, BCL-2 and BCL-X L were compared between the six multiple-myeloma-derived cell lines most sensitive to S63845 (left, IC 50 < 10 nM; data extracted from Extended Data Table 1) and six least sensitive ones (right, IC 50 > 100 nM). For gel source images, see Supplementary Fig. 1.
Extended Data Figure 6 | Anti-tumour efficacy and effect of dose
scheduling of S63845 in H929 and AMO1 multiple myeloma xenograft models. The in vitro activity of S63845 in human Burkitt-lymphoma-derived cell lines and in vivo activity of S63845 on individual E μ-Myc lymphoma cell lines. a , Anti-tumour effect of S63845 in H929 multiple myeloma xenograft models. Mean ± s.e.m. tumour volumes of eight animals per treatment group are shown (***P < 0.001 compared to vehicle). For tumour source data, see Supplementary Fig. 2. Tumour volumes of 8 individual mice per treatment group (shown in Fig. 2b) are shown. b , SCID mice were inoculated with 5 × 106 AMO1 cells and randomized nine days after grafting. After randomization, mice were either not treated (black line) or treated by i.v. administration of S63845, every day for 5 consecutive days at 25 mg per kg body weight (red line). For tumour source data, see Supplementary Fig. 2. c , Comparison of S63845 anti-tumour efficacy in the AMO1 model after administration at 25 mg per kg body weight either twice a week for two weeks (red diamonds) or once a week for two weeks (orange triangles). Mean ± s.e.m. tumour volumes of eight animals per treatment group are shown (***P < 0.001 compared to vehicle). For tumour source data, see Supplementary Fig. 2. d , Body weight evaluation of mice that were either left untreated (black squares) or treated with S63845 at 25 mg per kg body weight twice a week for two weeks (red diamonds) or once a week for two weeks (orange triangles). Mean ± s.e.m. body weights of eight animals per treatment group are shown. For source data, see Supplementary Fig. 2. e , Sensitivity of human Burkitt-lymphoma (BL)-derived cell lines to S63845. IC 50 values of Burkitt-lymphoma-derived cell lines were determined following 24 h in vitro exposure to increasing doses of S63845. Average IC 50 values were determined from three biological replicates (each carried out in triplicate, see source data); s.d. are shown. f , Representative haematoxylin and eosin (H&E)-stained sections of spleens and bone marrow from mice transplanted with E μ-Myc lymphoma cells 4 days after the end of treatment with either vehicle or S63845 from Fig. 2e. Scale bars represent 553 μm for the ×5 objective, 272 μm for the ×10 objective, 133 μm for the ×20 objective and 68 μm for the ×40 objective. g , Response of different E μ-Myc lymphoma-derived cell lines to in vivo treatment with S63845. Survival curves of C57BL/6–Ly5.1+ mice transplanted with each of the six independent E μ-Myc lymphoma-derived cell lines that were treated on days 5–9 after transplant with either vehicle (black line) or 25 mg per kg body weight S63845 (red line), by tail vein injection (see source data). A composite of the data from all of these E μ-Myc lymphoma-derived cell lines is presented in Fig. 2e.
Extended Data Figure 7 | Spearman correlations distribution in haematological cell lines and AML data on patient samples. a, Waterfall plots on Spearman correlations between human transcriptome (RNA- seq gene FPKM from CCLE database) and S63845 pIC50 (pIC50 =
?l og10(IC50)) measured on a panel of 24 haematological cancer-derived cell lines. Raw P values were adjusted for multiple testing using Benjamini-Hochberg correction. Only correlations with false discovery rate (FDR) <0.05 were retained for the analysis. Spearman correlations were ranked and plotted as a distribution. The threshold was set at r=0.4, which corresponded to half of the maximum correlation. b, S63845 activity against primary AML samples relative to comparable drugs. Cell viability was assessed by flow cytometric enumeration of Sytox Blue-negative cells after gating on blast cells. The concentration of each drug (in μM) causing 50% lethality for each sample (LC50) is shown. Cytogenetic risk for each sample is defined as intermediate (I) or adverse (A). NA indicates not available. Cell viability (%) after 48 h of treatment with vehicle is also shown. c, AML cell colony-forming assays showing clonogenic capacity
of CD34+ sorted cells from two G-CSF mobilized normal, healthy donors (red lines and filled circles) and primary samples from 3–6 patients with AML (black symbols and lines) after 14–21 days exposure to S63845, ara-C or idarubicin, normalized to vehicle control. Error bars show ±s.d.of
colony counts from duplicate plates (see source data).
Extended Data Figure 8 | S63845 activity in solid tumour-derived
cell lines, correlation with BCL-X L mRNA expression and impact of treatment with the MEK1/2 inhibitor, trametenib, the HER-2 inhibitor, lapatinib, the B-RAF inhibitor, PLX-4032, or the EGFR inhibitor, tarceva, on the levels of p-ERK and the pro-apoptotic protein BIM. a, Viability of NSCLC-, melanoma- and breast tumour-derived cell lines treated with S63845. Sensitive cell lines (IC50<0.1μM) are indicated in red, moderately sensitive cell lines (0.1 μM1μM) in green. Mean IC50 and individual data points from n=2 biological replicates are shown (see source data). b, The impact of the BCL-X L mRNA expression levels on the sensitivity of a panel of 110 solid tumour-derived cell lines to S63845 (see source data). BCL-
X L mRNA expression levels (RNA-seq) were extracted from the CCLE database. The Pearson correlation coefficient and P value are shown. c, Waterfall plots on Spearman correlations between human transcriptome (RNA-seq Gene FPKM from CCLE database) and S63845 pIC50 measured on a panel of 110 solid tumour cell lines. Raw P values were adjusted for multiple testing using Benjamini-Hochberg correction. Only correlations with FDR <0.05 were retained for analysis. Spearman correlations were ranked and plotted as a distribution. The threshold was set at r=0.4, which corresponded to half of the maximum correlation. d, Tumour cells were incubated with the indicated inhibitors for 16 h, before assessing the protein levels of BIM, ERK, phosphorylated (that is, activated) ERK (P-ERK) and actin (used as a protein loading control) by immunoblotting. For gel source images, see Supplementary Fig. 1. e, SK-MEL-28 cells were treated with S63845 with or without further addition of the MEK1/2 inhibitor, trametenib. Data are normalized to baseline cell survival at the time of initial drug treatment (day 0). Mean and individual data points
from three biological replicates are shown (see source data).
Extended Data Figure 9 | Tolerability of S63845 in mice and impact of treatment on healthy tissues at doses that prevent tumour expansion. a , Impact of treatment with S63845 at doses that prevent tumour
expansion on healthy tissues in mice. Healthy (not tumour-burdened) C57BL/6–Ly5.1+ mice were treated for 5 consecutive days with either vehicle or 25 mg per kg body weight S63845, and analysed 3 days after treatment had finished. Student’s unpaired t -test was carried out to compare the organ weights of spleen, thymus, lymph nodes, liver and kidney between vehicle and drug-treated mice. The organ weights were not significantly altered in response to treatment with S63845 (see source data). b , Representative haematoxylin and eosin-stained sections of the heart, liver, muscle and kidneys taken from vehicle- or S63845-treated mice at day 9 following treatment for 5 days (days 1–5). Scale bars represent 112 μ m for the × 20 objective and 57 μ m for the ×40objective.c , Impact of treatment with increasing doses of S63845 on C57BL/6 mice. Kaplan–Meier survival curves are shown for mice treated with vehicle or
with 25, 40, 50 or 60 mg per kg body weight S63845 for 5 consecutive days (see source data). There were 3 female and 3 male 7–8-week-old mice in each treatment group (except for the 40 mg per kg group where n =5because one mouse from this treatment group had to be killed owing to an injury incurred during drug administration). Using a Mantel–Cox test only the 60 mg per kg body weight dose showed significant changes relative to treatment with vehicle, * * * P =0.0006.d , Blood cell count analysis of the mice described in b (see source data). The mice were
analysed as they were killed, or for the mice surviving the entire treatment, 3 days after the 5 day-treatment had been completed. Unpaired two-tailed t -test was performed and compared to vehicle. For PLT counts, compared to vehicle, * * P = 0.0027 for the 25 mg kg dose, * * * P = 0.0005 for the 40 mg per kg dose and * P = 0.0245 for the 50 mg per kg dose of S63845. For the RBC counts, compared to vehicle, * P = 0.0312 for the 50 mg per kg dose and * P = 0.0242 for the 60 mg per kg dose of S63845.
Extended Data Table 1 | Data collection and refinement statistics
a Values in parentheses are for the highest-resolution shell.
英语阅读系列·有趣的字母
攀登英语阅读系列·有趣的字母 北京师范大学“认知神经科学与学习”国家重点实验室攀登英语项目组编著 Lesson1 Frank the Rat 大老鼠弗兰克Frank the rat is in a bag. 大老鼠弗兰克在袋子里呢。 Frank is in a hat. 他在圆顶帽子里呢。 Frank is in a pan. 他在平底锅里呢。 Frank is on an apple. 他在苹果上呢。 Frank is on a bat. 他在球棒上呢。 “Oh, no!” Frank is on a cat. “噢,糟了!”弗兰克落在了猫身上! Lesson 2 The Biscuits 我们来做饼干“I’m hungry!”“我饿了!” A biscuit…一块饼干可以是...... A biscuit can be a bus. 一块饼干可以是公共汽车。 A biscuit can be a bike. 和一块饼干可以是自行车。 A biscuit can be a boat. 一块饼干可以是小船。 A biscuit can be a banana. 一块饼干可以是香蕉。
A biscuit can be a bear. 一块饼干可以是小熊。 A biscuit can be a butterfly. 一块饼干可以是蝴蝶。 But…If birds are nearby…但是…..如果小鸟恰好在旁边的话…… The biscuits can only be birds.饼干就只是小鸟啦。 Lesson 3 Cool Cat 酷猫卡里 Cary is a cool cat. 卡里是只酷酷的小猫。 Cary can cut carrots like this. 卡里能像这样切胡萝卜。 Cary can climb a coconut tree like this. 卡里能像这样爬树。 Cary can clean a crocodile like this. 卡里能像这样清理鳄鱼。 Cary can catch flies like this. 卡里能像这样抓苍蝇。 Can Cary color like this? 卡里能像这样涂色吗? Yes! Cary is a cool cat. 是的!卡里是只酷酷的小猫。 Lesson 4 Dancing Dad 爸爸爱跳舞
一年级攀登英语一级A教学计划 一年级攀登英语一级A教学计划 1、激发学生学习英语的兴趣,培养他们学习英语的积极态度,使他们初步建立学习英语的自信心。 2、培养学生具有一定的语感和良好的语音、语调及书写基础,以及良好的学习习惯。 3、培养学生的观察、记忆、思维、想象和创造能力。 一年级攀登英语一级A教学计划 (20**学年度第一学期) 本学期我担任一年级4个班的攀登英语教学工作,现我对本学期教学工作做如下计划: 一、学生情况分析 一年级的孩子的年龄多为6周岁,具有好奇、好活动、爱表现、善模仿等特点。他们的学习兴趣很浓,接受能力、模仿能力很强,学习习惯初步养成,因此在本学期应注重培养学生良好的学习习惯,训练学生的听说能力,调动他们的自主能动性、积极性,营造互帮互助,共同学习英语的语境。 二、教学目标 1、激发学生学习英语的兴趣,培养他们学习英语的积极态度,使他们初步建立学习英语的自信心。 2、培养学生具有一定的语感和良好的语音、语调及书写基础,以及良好的学习习惯。
3、培养学生的观察、记忆、思维、想象和创造能力能在图片、手势、情境等非语言提示的帮助下,听懂清晰的话语和录音。 三、教材分析 本书共由五部分构成:本册教材学习内容包括:日常英语(Everyday English)、歌曲童谣(Songs and Chants).动画英语(Cartoon English)等 1、日常英语:与学生日常生活密切相关的情景对话,共12个话题,每个话题包括2-4句情景对话。 2、动画英语:以《迪士尼神奇英语》(上)VCD为基本学习材料。 共6张VCD,12课,每课4个小节,由学生熟悉和喜欢的迪士尼动画片片段组合而成。 3、歌曲童谣:包括歌曲和童谣两大块,其中有精心制作的传统英文经典歌曲,也有攀登英语独创的童谣日常英语替换内容:以日常英语重 点句型为主线,结合歌曲童谣和动画英语中高频出现的词汇进行的开放性交替。 5、节奏英语:将日常英语替换内容编成12段朗朗上口的韵文,并 配以节奏明快的背景音乐形成的独特学习内容。 四、教学措施 1、考虑到小学生好动爱玩的特点,以活动为课堂教学的主要形式,设计丰富多彩的教学活动,让学生在乐中学、学中用,从而保证学生英 语学习的可持续性发展。 2、通过听、说、读、写、唱、游、演、画、做等形式,进行大量 的语言操练和练习。
攀登英语阅读系列·有趣的字母 北京师范大学“认知神经科学与学习”国家重点实验室攀登英语项目组编著 Lesson1Frank the Rat 大老鼠弗兰克 Frank the rat is in a bag. 大老鼠弗兰克在袋子里呢。 Frank is in a hat. 他在圆顶帽子里呢。 Frank is in a pan. 他在平底锅里呢。 Frank is on an apple. 他在苹果上呢。 Frank is on a bat. 他在球棒上呢。 “Oh, no!” Frank is on a cat. “噢,糟了!”弗兰克落在了猫身上! Lesson 2 The Biscuits 我们来做饼干 “I’m hungry!”“我饿了!” A biscuit…一块饼干可以是...... A biscuit can be a bus.一块饼干可以是公共汽车。 A biscuit canbe a bike. 和一块饼干可以是自行车。 A biscuit can be a boat. 一块饼干可以是小船。 A biscuit can be a banana. 一块饼干可以是香蕉。 A biscuit can be a bear. 一块饼干可以是小熊。 A biscuit can be a butterfly. 一块饼干可以是蝴蝶。 But…If birds are nearby…但是…..如果小鸟恰好在旁边的话…… The biscuits can only be birds.饼干就只是小鸟啦。 Lesson 3 Cool Cat 酷猫卡里 Cary is a cool cat. 卡里是只酷酷的小猫。 Cary can cut carrots like this. 卡里能像这样切胡萝卜。 Cary can climb a coconut tree like this. 卡里能像这样爬树。 Cary can clean a crocodile like this. 卡里能像这样清理鳄鱼。 Cary can catch flies like this.卡里能像这样抓苍蝇。 Can Cary color like this? 卡里能像这样涂色吗? Yes! Cary is a cool cat. 是的!卡里是只酷酷的小猫。 Lesson 4 Dancing Dad 爸爸爱跳舞 Dad loves dancing! 爸爸爱跳舞! Dad is dancing with the desk. 他和桌子一起跳。 Dad is dancing with the duck. 他和鸭子一起跳。 Dad is dancing with the door. 他和门一起跳。 Dad is dancing with the dog. 他和小狗一起跳。 Dad is dancing with the deer. 他和小鹿一起跳。 Where is Dad? 爸爸在哪儿呀? Wow!哇! What a dancing Dad! 真是个爱跳舞的爸爸! Lesson 5 Red Ben 小本的红色世界 Ben likes red. 小本喜欢红色。 Ben paints the eggs red. 他把鸡蛋涂成红色。 Ben paints the eggplants red. 他把茄子涂成红色。 Ben paints the lemons red. 他把柠檬涂成红色。
攀登英语——有趣的字母 A: Frank the rat 老鼠弗兰克 Frank the rat is in a bag. 大老鼠弗兰克在袋子里。 Frank is in a hat. 弗兰克在圆顶帽子里。 Frank is in a pan. 弗兰克在平底锅里。 Frank is on an apple. 弗兰克在苹果里。 Frank is on a bat. 弗兰克在球棒上。 “Oh/no!”F r ank is on a cat. “哦?不!”弗兰克落在了猫身上。 B:The Biscuits 饼干 “I’m h ungry!”“我饿了!” A biscuit, —块饼干 A biscuit can be a bus. —块饼干可以是公共汽车。 A biscuit can be a bike. 可以是自行车。 A biscuit can be a boat. 可以是船。 A biscuit can be a banana. 可以是香蕉。 A biscuit can be a bear.可以是小熊。 A biscuit can be a butterfly.可以是蝴蝶。 But,if birds are nearby,但是,如果鸟儿靠近 The biscuits can only be birds.饼干只能是小鸟啦。 C: Cool Cat酷猫卡里 Cary is a cool cat.卡里是只酷酷的小猫。 Cary can cut carrots like this.卡里能像这样切胡萝卜。 Cary can climb a coconut tree like this. 卡里能像这样爬树。Cary can clean a crocodile like this.卡里能像这样淸洁鳄鱼。Cary can catch flies like this.卡里能像这样抓苍蝇。 Can Cary color like this? 卡里能像这样涂色吗? Yes!是的 Cary is a cool cat.卡里是只酷酷的小猫。 D: Dancing Dad爸爸爱跳舞 Dad loves dancing!爸爸爱跳舞! Dad is dancing with the desk.他和桌子一起跳。
攀登英语-有趣的字母(中英文_纯文字_26 篇全)
攀登英语——有趣的字母 A: Frank the rat 老鼠弗兰克 Frank the rat is in a bag. 大老鼠弗兰克在袋子里。 Frank is in a hat. 弗兰克在圆顶帽子里。 Frank is in a pan. 弗兰克在平底锅里。 Frank is on an apple. 弗兰克在苹果里。 Frank is on a bat. 弗兰克在球棒上。 “Oh/no!”F r ank is on a cat. “哦?不!”弗兰克落在了猫身上。 B:The Biscuits 饼干 “I’m h ungry!”“我饿了!” A biscuit, —块饼干 A biscuit can be a bus. —块饼干可以是公共汽车。 A biscuit can be a bike. 可以是自行车。 A biscuit can be a boat. 可以是船。 A biscuit can be a banana. 可以是香蕉。 A biscuit can be a bear.可以是小熊。 A biscuit can be a butterfly.可以是蝴蝶。 But,if birds are nearby,但是,如果鸟儿靠近 The biscuits can only be birds.饼干只能是小鸟啦。 C: Cool Cat酷猫卡里 Cary is a cool cat.卡里是只酷酷的小猫。 Cary can cut carrots like this.卡里能像这样切胡萝卜。 Cary can climb a coconut tree like this. 卡里能像这样爬树。Cary can clean a crocodile like this.卡里能像这样淸洁鳄鱼。Cary can catch flies like this.卡里能像这样抓苍蝇。 Can Cary color like this? 卡里能像这样涂色吗? Yes!是的 Cary is a cool cat.卡里是只酷酷的小猫。 D: Dancing Dad爸爸爱跳舞 Dad loves dancing!爸爸爱跳舞! Dad is dancing with the desk.他和桌子一起跳。 Dad is dancing with the duck.他和鸭子一起跳
英语阅读系列·有趣的字母 攀登英语阅读系列?有趣的字母 攀登英语阅读系列·有趣的字母 北京师范大学“认知神经科学与学习”国家重点实验室攀登英语项目组编著 Lesson1 Frank the Rat 大老鼠弗兰克 Frank the rat is in a bag. 大老鼠弗兰克在袋子里呢。
Frank is in a hat. 他在圆顶帽子里呢。Frank is in a pan. 他在平底锅里呢。Frank is on an apple. 他在苹果上呢。Frank is on a bat. 他在球棒上呢。“Oh, no!” Frank is on a cat. “噢,糟了!”弗兰克落在了猫身上! Lesson 2 The Biscuits 我们来做饼干 “I'm hungry!”“我饿了!” A biscuit…一块饼干可以是...... A biscuit can be a bus. 一块饼干可以是公共汽车。 A biscuit can be a bike. 和一块饼干可以是自行车。 A biscuit can be a boat. 一块饼干可以是小船。 A biscuit can be a banana. 一块饼干可以是香蕉。. 攀登英语阅读系列?有趣的字母 A biscuit can be a bear. 一块饼干可以是小熊。 A biscuit can be a butterfly. 一
块饼干可以是蝴蝶。 But…If birds are nearby…但是…..如果小鸟恰好在旁边的话…… The biscuits can only be birds.饼干就只是小鸟啦。 Lesson 3 Cool Cat 酷猫卡里 Cary is a cool cat. 卡里是只酷酷的小猫。 Cary can cut carrots like this. 卡里能像这样切胡萝卜。 Cary can climb a coconut tree like this. 卡里能像这样爬树。 Cary can clean a crocodile like this. 卡里能像这样清理鳄鱼。 Cary can catch flies like this. 卡里能像这样抓苍蝇。 Can Cary color like this? 卡里能像这样涂色吗? Yes! Cary is a cool cat. 是的!卡里是只酷酷的小猫。 爸爸爱跳舞Dancing Dad Lesson 4 攀登英语阅读系列?有趣的字母
攀登英语——有趣的字母 A:Franktherat老鼠弗兰克 Franktheratisinabag.大老鼠弗兰克在袋子里。Frankisinahat.弗兰克在圆顶帽子里。 Frankisinapan.弗兰克在平底锅里。 Frankisonanapple.弗兰克在苹果里。 Frankisonabat.弗兰克在球棒上。 “Oh/no!”F rankisonacat.“哦?不!”弗兰克落在了猫身上。 B:TheBiscuits饼干 “I’mhungry!”“我饿了!” Abiscuit,—块饼干 Abiscuitcanbeabus.—块饼干可以是公共汽车。Abiscuitcanbeabike.可以是自行车。 Abiscuitcanbeaboat.可以是船。 Abiscuitcanbeabanana.可以是香蕉。 Abiscuitcanbeabear.可以是小熊。Abiscuitcanbeabutterfly.可以是蝴蝶。 But,ifbirdsarenearby,但是,如果鸟儿靠近Thebiscuitscanonlybebirds.饼干只能是小鸟啦。 C:CoolCat酷猫卡里 Caryisacoolcat.卡里是只酷酷的小猫。Carycancutcarrotslikethis.卡里能像这样切胡萝卜。Carycanclimbacoconuttreelikethis.卡里能像这样爬树。Carycancleanacrocodilelikethis.卡里能像这样淸洁鳄鱼。Carycancatchflieslikethis.卡里能像这样抓苍蝇。CanCarycolorlikethis?卡里能像这样涂色吗? Yes!是的 Caryisacoolcat.卡里是只酷酷的小猫。 D:DancingDad爸爸爱跳舞 Dadlovesdancing!爸爸爱跳舞!Dadisdancingwiththedesk.他和桌子一起跳。